Health care network maturity model: How mature is YOUR organization?
Sign up for news and updates in population health
Jul 15, 2013
Time and tide wait for no man At Philips, we have the opportunity to work with a large number of organizations across the country, and in order to help us better understand our clients (and our clients to better understand themselves!) we have developed a Network Maturity Model that I would like to introduce in this week’s Philips Blog. Health systems and physician organizations across the country are working very hard these days to keep up with quickly changing reimbursement and care delivery models. Some of these organizations are very large and well staffed, but they may still be struggling to implement the programs, processes, and technology they need to meet these new challenges. Other organizations are just getting started aligning with physicians, establishing governance, and even finding office space for the teams they are building. Others are somewhere between these two extremes. The following graphic is how we look at providers and their networks, and this image will be the basis for today’s discussion and subsequent related Philips blog posts.
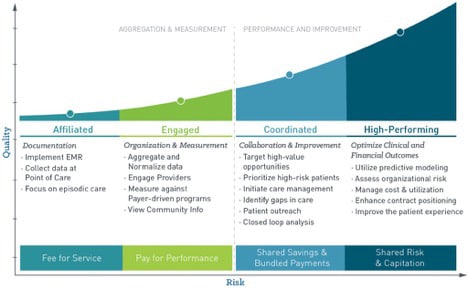
Progression to a higher-level of network maturity is a business imperative for all but the most mature networks, of which there are very few at this point in time. In this blog post, I’ll discuss what is driving the progression from Affiliated to Engaged to Coordinated and finally to High Performing.
Triple aim trifecta
Before we talk about WHY organizations are working to become High Performing Networks, let me devote a few sentences to WHAT a High Performing Network actually is. At a very macro level, High Performing Networks (or Narrow Networks as they are sometimes called) are those networks whose physicians and facilities are proactively and consistently meeting Triple Aim goals. There are a few subtly different definitions for The Triple Aim, but for this blog we’ll say that the High Performing Network has achieved the trifecta of high quality and lower cost care with high levels of patient satisfaction. These networks may be offering their services to payers or employers directly, which is one version of Accountable Care. That’s all easy to talk about and write about, but it takes a lot of resources and hard work to make it actually happen. We’ll cover some of those execution details in a future blog post.
The heart of the matter
The fundamental issue and driving force behind so many of the changes in health care these days is that our health care costs are out of control and the rate of rise in health care expenditure is unsustainable. This isn’t news. We’ve all seen the numbers like percentage of GDP spent on health care in the United States compared to other countries, but we can’t talk about what is driving Network Maturity without at least acknowledging that fundamental fact. Done. Part of the reason health care costs so much is because it is often inefficient, and health care providers (physicians and health systems both) are still generally paid for volume – not outcomes. That means there hasn’t been much focus on providing high quality care, which in the end can save money for payers and employers (lower complication rates, better disease prevention, fewer readmissions, etc.), even though it tends to cost more for physicians and their organizations to deliver.
Newer care delivery models are critical but costly
In order to focus on providing higher quality care, physicians and their organizations need to make significant changes to their processes. Care delivery models that can produce higher-quality care and greater Network Maturity, like The Patient Centered Medical Home (PCMH), The Chronic Care Model, Clinically Integrated Networks, etc. take a significant commitment to implement, and unless the incentives are in place this likely won’t happen. Why should physicians and their organizations financially support cost savings for payers and employers? They need some skin in the game, and until recently they really haven’t had enough of it.
Reimbursement models are foundational
Realizing that physicians and their networks won’t devote the resources needed to improve outcomes and reduce costs unless those investments are covered, the federal government and commercial payers have started changing the reimbursement models to incent physicians and their organizations to adopt newer care delivery models, transform the way they care for patients, and focus on process improvement. Reimbursement drives so much in health care. Let’s walk through some of these reimbursement models and discuss each one briefly. They are presented in increasing order of potential revenue and risk, although I purposefully left out Fee For Service and Full Capitation.
Patient centered medical home uplifts
More and more payers are offering uplifts to physicians for E & M codes if the office has been certified by the payer as a PCMH. The uplifts are often in the range of 20% and help to offset the cost of implementing a PCMH.
Pay-for-Performance (P4P or PFP)
PFP programs have been around for years, and they have grown in number, value, and complexity with each passing year. Generally speaking, physicians are paid for providing preventive care and chronic disease management at or above a certain level of performance. Any given PFP program typically has many metrics, and a physician will typically receive all or none of the potential for a given metric based on his or her outcomes. PFP has traditionally been for primary care providers, but we’re seeing more and more specialty care PFP these days.
Accountable care - Bundled payments
Bundled payments can be a great way for an organization to dip its toe in the Accountable Care waters. Agreeing to accept a set reimbursement for a defined service, such as a knee replacement, provides one or more specific opportunities to focus on, which can increase the chance for success. If the service that is included is provided efficiently and with a low complication rate, then there can be a nice upside. (Note that I’m talking here and in the sections below about Accountable Care in general, not specifically about the Affordable Care Act and Medicare ACOs, although they are all related.)
Accountable care - Shared savings
Of the two main types of Accountable Care models, the Shared Savings model seems to be the most popular. In this model, providers and their organizations have the opportunity to share in any savings realized as a result of their work, however there is no insurance risk to the providers or their networks. Some programs do include a component of performance risk, much like a P4P program.
Accountable care - Shared risk
In this model, providers and their organizations have the opportunity to share in any savings, but they also accept some of the insurance risk. There is real downside potential with this model, and in order to do well you really need a High Performing Network!
Reimbursement critical mass
Any given Network might participate with some or all of the above types of reimbursement models with different payers and/or employers. This means that physicians and their organizations are more likely to have what I like to call Reimbursement Critical Mass, which is that minimum percentage of revenue that is tied to improving clinical and financial outcomes independent of volume-based payments. What is that number? Well, it varies. For the older physician who is planning to retire soon, that number might be quite high, whereas for the employed physician who isn’t directly responsible for his or her practice’s P&L that number might be a lot lower. In my experience, I generally put that number somewhere between 10 – 20%. Anything less than that, and the necessary investments in programs and transformation of care won’t likely happen.
Tune in next time
Physicians and their organizations are responding to new and changing reimbursement models, which are driving network sophistication and maturity. Many networks have reached Reimbursement Critical Mass, and they are building programs and implementing technology and processes to help them succeed. In future Philips Blog posts I’ll talk more about what type of programs, processes, and technology characterizes each type of network: Affiliated, Engaged, Coordinated, and High Performing. We’ll also discuss how each step along the Network Maturity Model is related to specific reimbursement models and how YOUR organization can prepare to take things to the next level. Stay tuned!
About the author

Paul D. Taylor, MD,
CMO, Philips
Paul D. Taylor is CMO for Philips PHM. Board-certified Internal Medicine physician and entrepreneur with experience developing industry-leading Value-Based Care and Population Health Management solutions and implementing clinical quality improvement programs and systems of care at the physician, physician group, physician organization, and community levels.
You are about to visit a Philips global content page
Continue