Take a closer look at positional OSA
Defining positional OSA
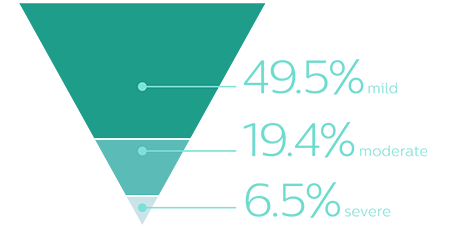
Positional OSA has been identified in many patients with OSA5
Positional OSA is a specific diagnosis in which the vast majority of apneic events occur during supine sleep.3 Positional OSA is diagnosed from any sleep study in which body position is measured. 47% of OSA patients may have exclusive positional OSA.4
Cartwright criteria uses the following to define and diagnose positional OSA3
AHIsupine ≥ 2 x AHInon-supine
Challenges and opportunities in treating positional OSA
Nonadherence with PAP therapies ranges from
29% - 83%
Addressing challenges with many available therapies
CPAP non-adherence ranges between 29-83%, when non-adherence is defined as a mean of less than or equal to 4 hours of use per night.6,7 Discover articles, news and information on positional OSA
An opportunity to optimize therapy
Targeted positional OSA therapy
Traditional sleep therapies used for OSA are also typically used to treat positional OSA, despite the availability of less invasive, validated treatments that target positional sleep apnea.
Data-driven results
Available therapies for positional OSA lack data feedback that allow for tracking treatment progress.
"Philips NightBalance can be a very unobtrusive way to manage the problem quite effectively."
Dr. Helene Emsellem
Center for Sleep and Wake Disorders
In treating your patients with positional OSA
We're on your side with a sleep therapy that makes a difference
Proven efficacy
The AHI during PSG on NightBalance was not importantly different from a clinical perspective to that on PAP therapy.1 The effectiveness of NightBalance and auto-adjusting positive airway pressure was similar across the categories of AHI severity.

Significantly higher adherence
Adherence with NightBalance was significantly higher than with PAP in patients diagnosed with positional OSA.1

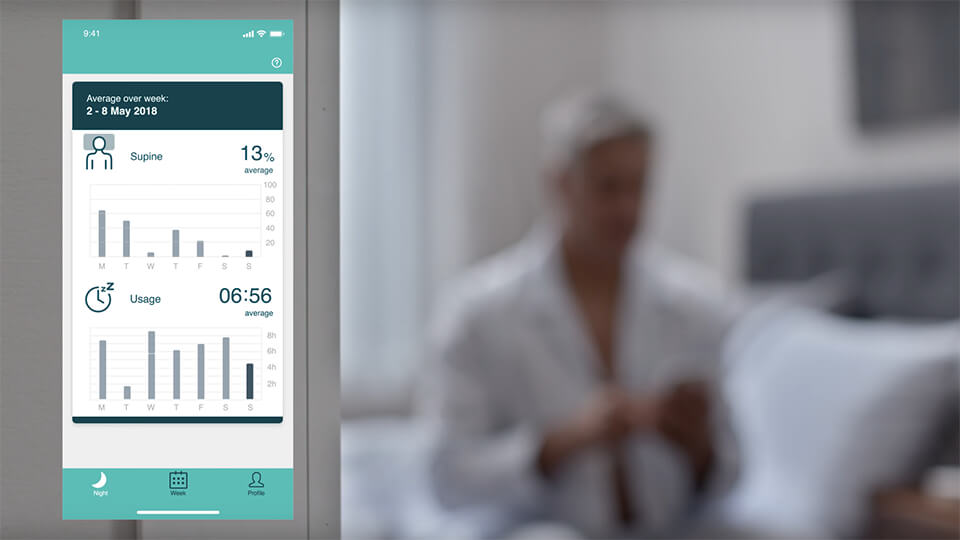
Data-driven results
Adherence and positional sleep data is accessible to you via a streaming, cloud-based system.
Backed by clinical evidence
NightBalance is supported by years of clinical studies in patients with positional OSA.
Berry, R. et al, NightBalance Sleep Position Trainer Device Versus Auto-Adjusting Positive Airway Pressure for treatment of Positional Obstructive Sleep Apnea Journal of Clinical Sleep Medicine, Vol. 5, No.7, 947-956
Van Maanen et al, The sleep position trainer: a new treatment for positional obstructive sleep apnoea Sleep and Breathing (2013) 17:771–779
Van Maanen & de Vries, Long-Term Effectiveness and Compliance of Positional Therapy with the Sleep Position Trainer
SLEEP 2014; Vol. 37, No. 7
Eijsvogel etal, Sleep Position Trainer versus Tennis Ball Technique
Journal of Clinical Sleep Medicine 2015; Vol. 11, No. 2
Dieljtens, A promising concept of combination therapy for positional obstructive sleep apnea
Sleep Breath 2015; 19:637–644
Benoist, Positional therapy in patients with residual positional obstructive sleep apnea after upper airway surgery
Sleep Breath 2016
Benoist, A randomized, controlled trial of positional therapy versus oral appliance therapy
Sleep Medicine 2017; 34:109e117
De Ruiter, Durability of treatment effects of the SPT versus oral appliance therapy in positional OSA: 12-month follow-up
Sleep Breath 2017
Laub, A Sleep Position Trainer for positional sleep apnea: a randomized, controlled trial
Journal of Sleep Research 2017
Better sleep with NightBalance

Exceptional comfort

Easy adjustment

More motivation
See how NightBalance is proven to make a difference
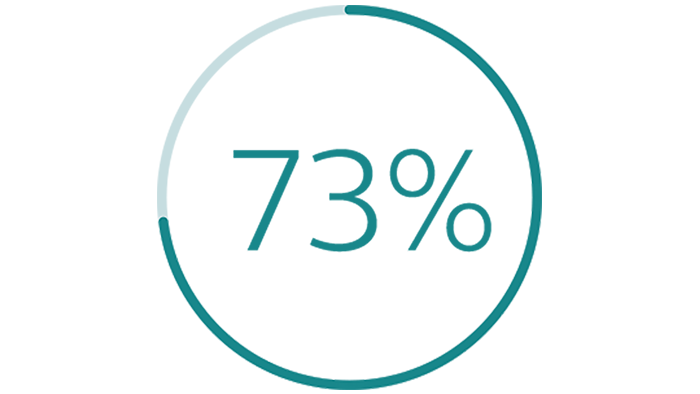
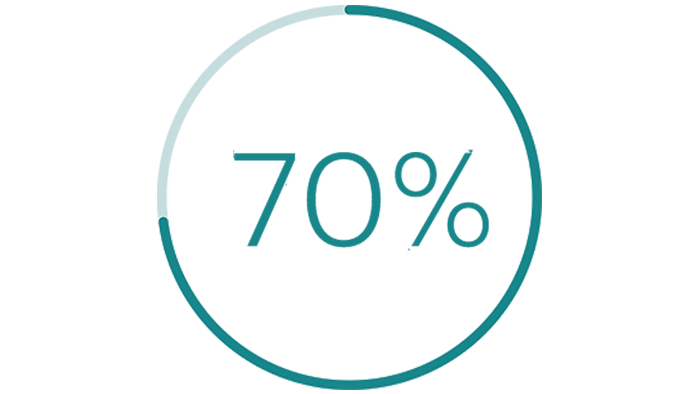
A survey following 75 NightBalance users for an average of 2.2 years reported impressive results.2
reported long-term improvement in the three most reported positional OSA symptoms (non-refreshing sleep, fatigue, episode of breathing cessations, gasping, and/or choking during the night)
reported feeling less sleepy during the day
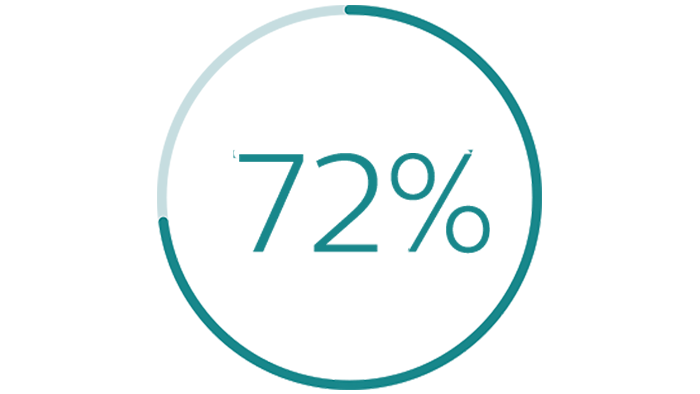
reported feeling more refreshed during the day
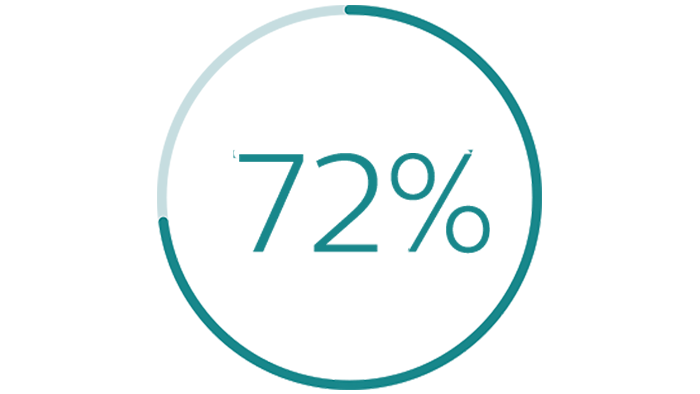
reported feeling a decrease in fatigue during the day
How it works
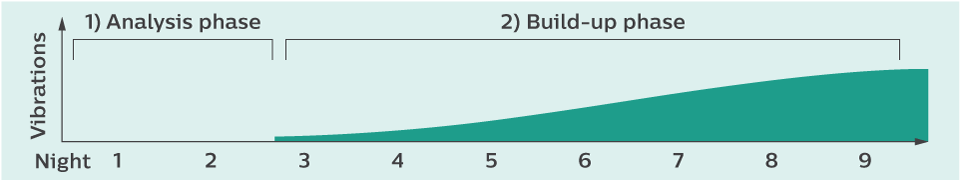
Analysis and build-up phases
NightBalance begins by analyzing sleep for the first two nights. It then gradually introduces gentle vibrations from night 3 through night 10 which are intended to acclimate the patient to the NightBalance device. Full therapy begins on night 10.
Nightly use
Patient can fall asleep in any position. After 15 minutes, the device activates and begins monitoring.

NightBalance detects when the patient is on their back. It prompts the patient to move off their back without disturbing their sleep.

Vibrations will stop when patient is on their side.
Resources
Sleep & Respiratory Newsletter
Brochures
Summary
Other
See how NightBalance works
No results near you?
Medical advisory board
NightBalance is supported by an our medical advisory board, comprised of distinguished world renowned scientists and clinicians.

Prof. Dr. Nico de Vries

David P. White, MD

Dr. Raphael Heinzer

Jean-Louis Pepin, MD, PhD

Prof. Dr. Winfried Randerath, MD
Winner, 2020 HME Business
new product award:
Sleep – Therapy Systems
Philips NightBalance

1 Berry, R. et al, NightBalance sleep position treatment device versus auto-adjusting positive pressure airway prssure for treatment of positional obstructive sleep apnea, J Clin Sleep Medicine,2019 ,Vol. 5, No.7, 947-956 2 NightBalance OSA Symptoms survey: Reimbursement Dossier Netherlands 3 Cartwright criteria, Effect of Sleep Position on Sleep Apnea Severity, R. Cartwright, 1984. 4 Heinzer, R. et al, Prevalence and Characteristics of Positional Sleep Apnea in the HypnoLaus Population-based cohort, Sleep Medicine 2018; 48:157-162. 5 Mador, J. et al, Prevalence of Positional Sleep Apnea in Patients Undergoing Polysomnography, Chest 2005, Volume 128, Issue 4, pages 2130-2137.6. Van Maanen et al. 2013, The sleep position trainer: a new treatment for positional obstructive sleep apnoea. 6 Sawyer, AM. et al, A systemic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions, Sleep Med Review, 2011 Dec, 15(6): 343-56 7 T. et al, Adherence to Continuous Positive Airway Pressure Therapy: the Challenge to Effective Treatment, Proceedings of the American Thoracic Society, Vol5, 2008 8 van Maanen, J. et al, The sleep position trainer: a new treatment for positional obstructive sleep apnoea, Sleep and Breathing, 2013, 17:771-779