In a patient with HIV and cardiovascular risk factors, MRI with Black Blood imaging helped to diagnose brain vasculitis. The same MRI protocol was later also used to noninvasively confirm treatment response. In this article, Niloufar Sadeghi MD, PhD, Neuroradiologist, Erasme Hospital, Brussels, Belgium provides clinical details on this case and insight into the utility of Black Blood imaging for diagnosis and treatment.

Dr. Sadeghi tells about a patient who presented in the Emergency Room at Erasme Hospital in Brussels, Belgium, with recurrent left leg weakness that had been occurring over a period of 24 hours. The patient was known to have been HIV-infected for four years, but was not treated for this infection. The patient had multiple cardiovascular risk factors such as obesity, glucose intolerance, arterial hypertension and hypercholesterolemia. The neurological examination showed left leg hemiparesis.
“After a conventional routine MR imaging examination, the suspicion of vasculitis arose, therefore we performed an MRI including Black Blood imaging in a separate session,” says Dr. Sadeghi. “The dedicated ExamCard includes diffusion, FLAIR, MR angiography using TOF ExamCard also includes Black Blood imaging before and after contrast. This examination was performed on our Ingenia 3.0T. Black Blood scan time 4:39 min, acquired voxel size 0.75 x 0.75 x 1.0 mm, 21 slices.”
On FLAIR images we can see some nonspecific high signal abnormalities in frontal white matter bilaterally. On DWI we can see acute ischemic lesions which appear with high signal intensity. Arrows show vessel wall enhancement which appears concentric and homogeneous in different cerebral territories.
“On the routine MR sequences that we did, we could see acute ischemic lesions. We see them very well on the diffusion images, where acute ischemic lesions usually appear with high signal intensity and restricted diffusion. However, the etiology of these lesions cannot be derived from these images.
An area of restricted diffusion was seen in the anterior cerebral artery territory and we concluded it was an ischemic lesion. On MR angiography we can just see if there is stenosis or vessel occlusion, but it does not provide us information on the etiology of this kind of lesion. So, we decided to perform Black Blood imaging. The presence and the pattern of vessel wall enhancement on Black Blood imaging can help us to determine the etiology of the lesion.
Many studies have shown that Black Blood imaging can help differentiate vasculitis from other causes of vasculopathy, such as atherosclerosis, with a high specificity [1-3]. In an atherosclerotic lesion, vessel wall thickening and enhancement are usually eccentric, while in vasculitis the wall thickening and enhancement are usually concentric, homogenous and in a long portion of the vessel. Furthermore, this imaging can also be used for the follow-up of patients whenever their treatment is installed in order to determine the efficacy of a particular treatment.
In this case the Black Blood imaging helped us to suggest the diagnosis of HIV-related brain vasculitis.
“With the multiple cardiovascular risk factors this patient had, such as glucose intolerance, arterial hypertension and hypocholesteremia, his lesions could be atherosclerotic lesions or vasculitis, conditions which require different treatment. Especially in this patient with HIV infection causing the vasculitis, treatment of the two conditions is different. The results of MRI with Black Blood imaging, helped to choose the preferred treatment for this patient, which was based on antiviral medication rather than an antiaggregant or anticoagulation treatment which is usually given to patients with risk of ischemia based on atherosclerotic lesions.
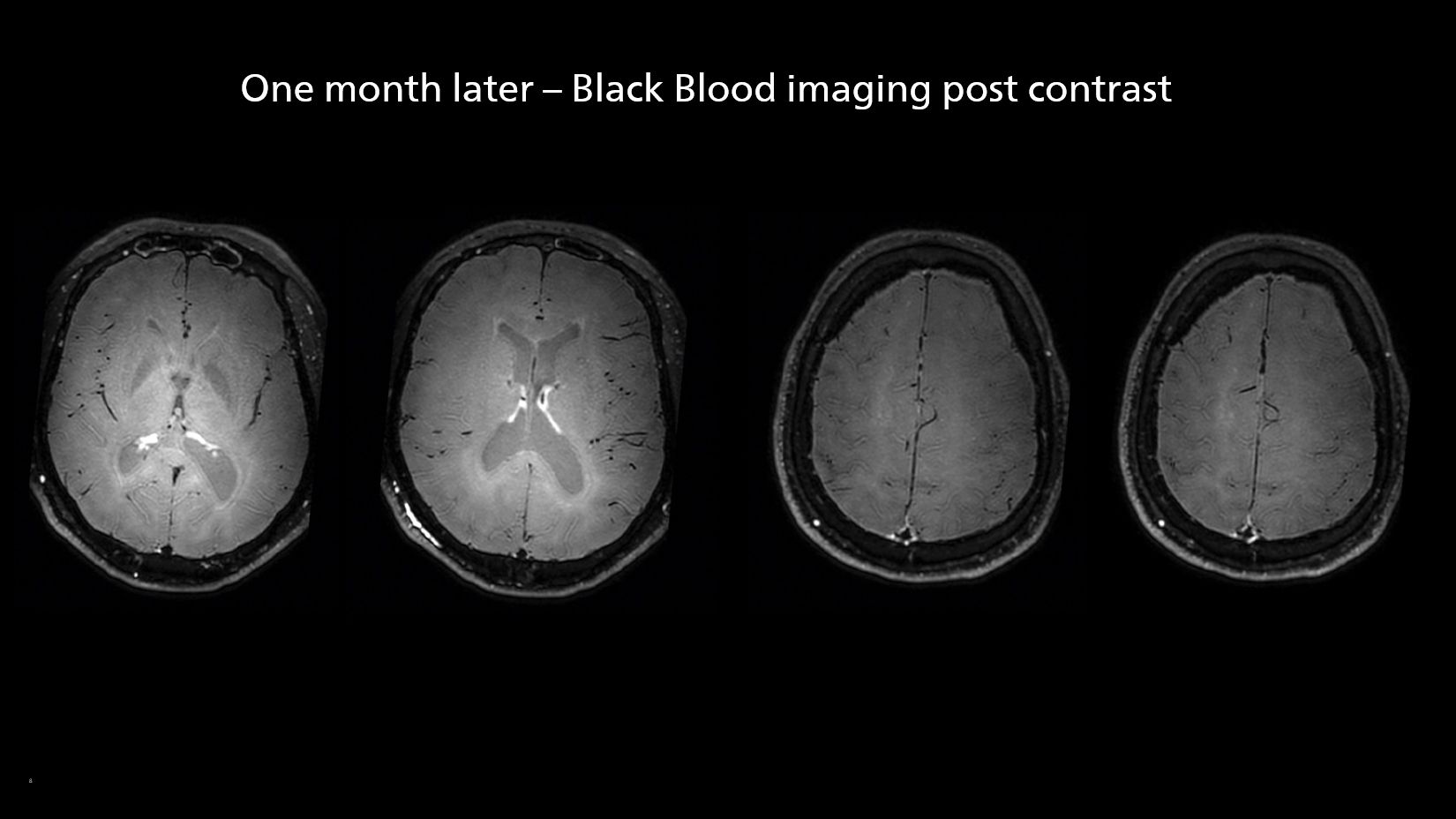
One month after beginning the antiviral treatment, the same MRI examination was repeated and again eight months after the beginning of treatment. On follow-up images, we see the enhancements have almost disappeared. So in case of this patient, the MRI exam with Black Blood imaging helped us to give the patient the appropriate treatment and also allowed us to noninvasively confirm the treatment response.”
After one month of treatment, post-contrast Black Blood images at the exact same levels as in the figure above show disappearance of the vessel wall enhancements which were seen on the previous examination.
Black Blood imaging can help us to noninvasively visualize vessel wall thickening and enhancement patterns that occur in vasculitis and help us distinguish it from atherosclerotic lesions. Imaging techniques such as time-of-flight (TOF) MR angiography are not very sensitive or specific for this kind of lesions. Other possible diagnostic methods are intra-arterial angiography or brain biopsies which are both invasive.
We do not perform this examination with Black Blood imaging on all patients with ischemic lesions in the brain, because in most patients the lesion origin is embolic or atherosclerotic. We typically use it in young patients (less than 60 years old) or those patients without cardiovascular risk factors. We find it important to use Black Blood imaging in such cases, because treatment is different for a patient with vasculitis.

Niloufar Sadeghi MD, PhD is neuroradiologist at Erasme Hospital in Brussels, Belgium since 2000. She completed her PhD in 2010 and has been recently nominated as professor.
