
MRI boosts treatment quality and patient experience in radiotherapy
In its ongoing mission to provide the highest quality patient care in the greater Geneva area, private healthcare provider Hôpital de La Tour (Switzerland) expanded its practice with a new oncology center offering medical oncology and radiotherapy services. Physicist Grégory Bolard was determined to make MRI accessible for precise radiotherapy planning for La Tour’s radiotherapy patients. His team’s ambition was to adopt MR simulation to better delineate targets and identify OARs, and to streamline the MR-based planning process via MR-only radiotherapy planning.

MRI boosts treatment quality and patient experience in radiotherapy
Mr. Bolard was hired to launch the entire radiotherapy department from the ground up: planning the physical space, putting the RT team in place and equipping the department with all necessary technology.
“With all high-end technology and treatment techniques at the linac’s side, we can target the radiation dose very accurately,” Mr. Bolard says. “But in many cases, target delineation is the largest uncertainty in the treatment process. To increase our confidence in the delineation steps, it was obvious that we should have access to an MRI simulator.
“La Tour’s administration and clinicians appreciated that MRI is a must-have for modern radiotherapy,” he says. “So, they agreed to acquire an MRI scanner – an Ingenia MR-RT – which would be shared between radiology and radiation therapy.” The radiotherapy department now offers MR simulation to all patients eligible and anatomies include brain, prostate, rectum, anal cancer, head/neck and gynecological cancers.
Patient well-being is a central theme in our department
“Patient well-being is a central theme in our department,” Mr. Bolard says. “A radiotherapy department can be a gloomy environment in the absence of natural light. It was a ‘must-have’ for us in order to create a warm and calming atmosphere. Working with Philips we created a plan to bring light to the different imaging rooms and waiting areas. So, we have Ambient Experience on the MR and CT simulators, as well as on the PET-CT. The patients appreciate it a lot, because it decreases stress and anxiety.

Philips CT Big Bore and Ingenia MR-RT rooms are equipped with Ambient Experience.
The radiotherapy department at Hôpital de La Tour, Meyrin, Switzerland has access to the following systems:

This shared-use model has made MRI economically affordable for us
The MR scanner is located in the adjacent radiology wing and the radiotherapy department receives two dedicated slots per week, amounting to three hours total for patients eligible for MR simulation.
“This is an ideal situation for us,” Mr. Bolard says. “With our patient load of about 300 patients each year, having our own MRI system was unrealistic. This shared-use model has made MRI economically affordable for us.”
The collaboration between the two departments has been vital. “Clinicians in both departments appreciate the need for high quality imaging for RT planning and diagnostic purposes, and work together cooperatively to make that a reality,” Mr. Bolard says.
Hôpital de La Tour manages an efficient radiotherapy service with a limited staff in key roles: 4.7 FTE radiation therapy technologists (RTTs), 1.8 FTE physicists, 2 radiation oncologists and 2 FTE administrative staff. The team enthusiastically accepted the challenge to implement MRI. The first step was to get information from other, more experienced sites.
Therefore, Mr. Bolard and Thomas Breuneval, MD, a radiation oncologist at Hôpital de La Tour, attended a Philips-organized peer-to-peer course at University Medical Center Utrecht (UMC Utrecht), Netherlands to gain expert knowledge on MRI implementation.
Particularly as a small center, it is essential to learn from others, Dr. Breuneval recalls. “UMC Utrecht shared some valuable technical tools and their clinical best practices with us that helped speed up implementation at La Tour. And the extensive MRI experience of UMC Utrecht helped us increase our understanding of how to use the images, as well as which sequences to use and how these influence target delineation.”
Integrating MRI in the radiotherapy workflow for our head-and-neck cancer patients was a logical step for La Tour’s new radiotherapy department, Mr. Bolard says.
“We have an excellent head-and-neck cancer program here that attracts many patient referrals from the larger Geneva region,” he says. “Our radiation oncologists decided to introduce MR-sim for head-and-neck cases to provide much more definitive soft tissue images than what CT can provide.”
While CT clearly defines bone and cartilage, the modality’s limited soft tissue visualization makes head-and-neck structures often appear virtually indistinguishable from another. Coregistering an MRI dataset as a secondary information source for head-and-neck target and organ at risk (OAR) delineation is vital, according to La Tour’s Dr. Breuneval.
“MRI contributes substantially to visualizing head-and-neck lesions compared to CT and allows a better differentiation of normal from abnormal tissue,” he explains. “Tumor edges and extracapsular lymph node extension – as well as OARs, such as parotid glands, pharyngeal muscles and the brachial plexus – are better depicted. The resulting benefit is that tumor margins may be reduced and OARs better spared.”

To facilitate accurate CT-MRI co-registration, the La Tour team connects a 5-point CIVCO FreedomView thermoplastic mask directly onto the Philips couch top (left). The dStream Anterior coil and Flex L coils are used for high quality imaging (right).
The patient was diagnosed with an epidermoid carcinoma of the base of the left invading the amygdala lodge and the amygdaloglossal groove. Radiochemotherapy with curative aim was prescribed with a dose of 70 Gy for the tumor, 66 Gy on the suspicious nodes and 56 Gy on the elective drainage areas - in 33 fractions.
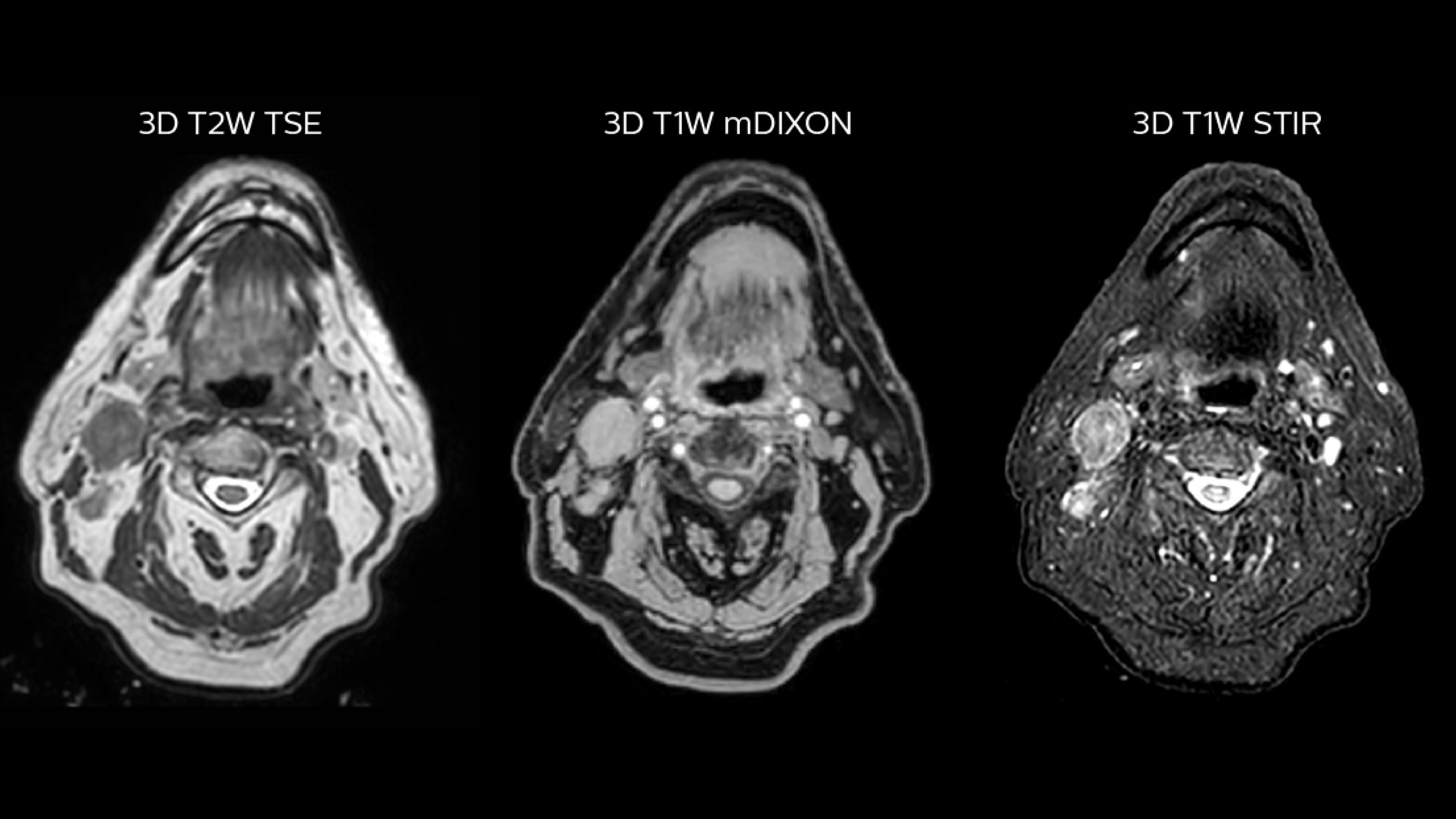
T2W 3D (left), 3D STIR (center) and mDIXON (right) MRI scans.
Simulation imaging:

Comparison of CT simulation scan (left) and T2W 3D MRI (right)
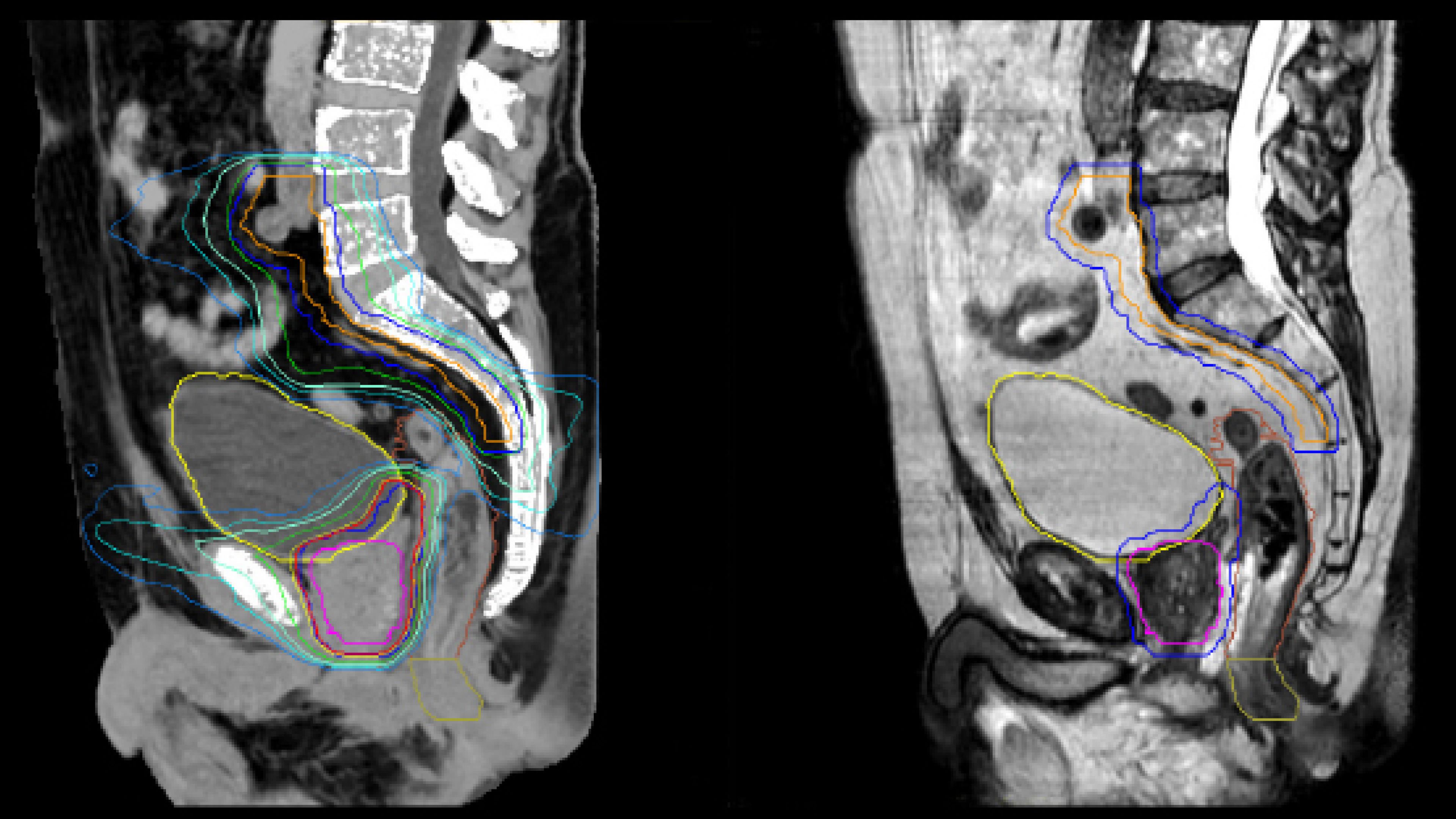
MR-based contouring and planning: MR-based target contouring on 3D T2W TSE in transversal, sagittal and coronal planes.

MR-based target contouring in transversal, sagittal and coronal planes.
MR-based contouring and planning:
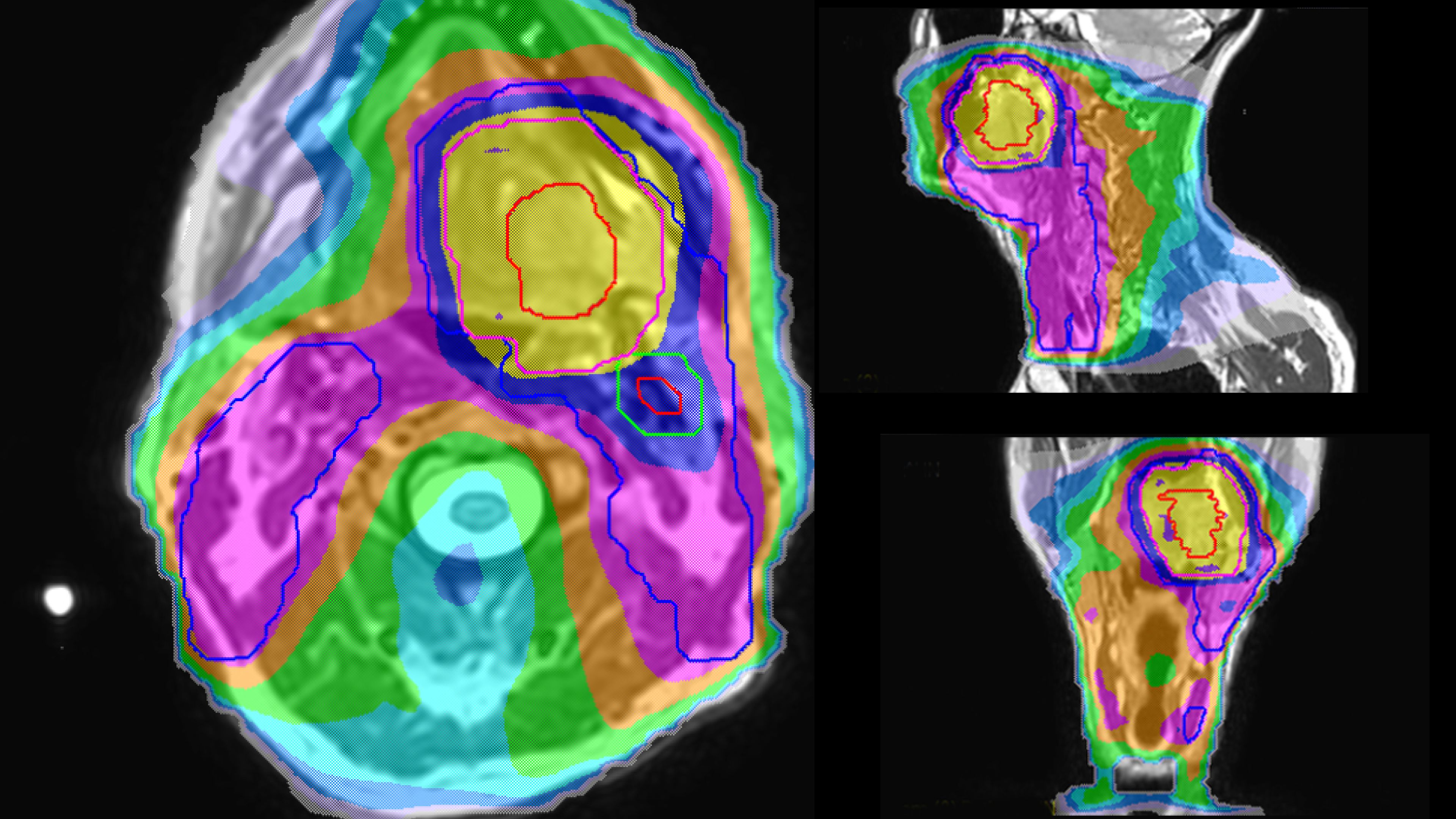
Personalized VMAT dose planned in Philips Pinnacle.
As a private institution we aim to offer both the best treatment and the best patient experience. MR only radiotherapy makes so much sense in this respect.
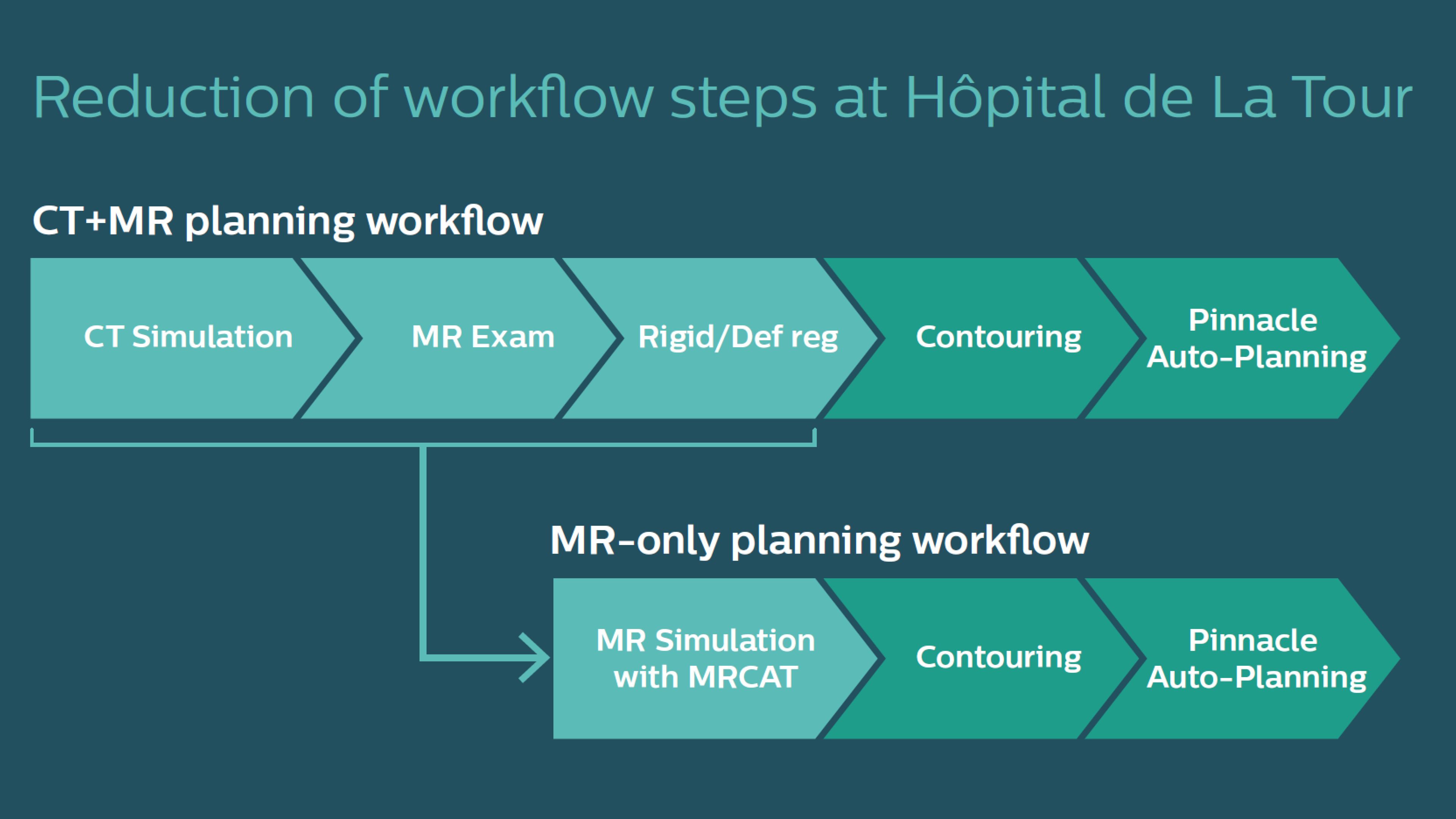
When MR-only radiotherapy planning is performed, no CT simulation of the patient is needed. Even from the start, there was no doubt that Hôpital de La Tour was going to provide MR-only radiotherapy planning for their pelvic cancer patients.
“As a private institution we aim to offer both the best treatment and the best patient experience,” Mr. Bolard says. “MR-only radiotherapy makes so much sense in this respect. Referring physicians also totally appreciate the rationale for using MRI, as they are very familiar with MRI for diagnosis. And the fact that we can save the patient from undergoing multiple exams is a big advantage and a driver for patient referrals.”
Philips MRCAT (MR for Calculating ATtenuation) provides exceptional soft tissue contrast for target and OAR delineation, in addition to the Hounsfield units needed for dose calculations. This permits an MR-only radiotherapy planning workflow. Philips pioneered MR-only radiotherapy with the introduction of MRCAT Prostate, followed by the expansion to the whole pelvis with MRCAT Pelvis. This application can be used for a broad range of pelvic indications, including cancers in the prostate, rectum, bladder, anal canal and cervix. Next to MRCAT Pelvis, MRCAT Brain is available for radiotherapy planning of primary and metastatic soft-tissue tumors in the brain.
Before clinical use of MR-only radiotherapy planning, the team completed a commissioning project to confirm dosimetric accuracy of the MRCAT approach.
“In my previous hospital, we commissioned MRCAT Prostate by performing a small-scale clinical study [2,3] that compared CT-sim versus MRCAT on our Ingenia 3.0T MR-RT system,” Mr. Bolard says. “The results were very good; the MRCAT-based dose calculations resembled the CT-based calculations. After that study, we started applying MRCAT Prostate in clinical routine.”
Before introducing MRCAT Pelvis at La Tour, Mr. Bolard and his colleague, radiation oncologist Ambroise Champion, MD, conducted a validation study on their first 43 pelvic patients (32 prostate, 9 rectum, 1 bladder, 1 anal canal).
“Instead of doing a separate CT-sim initially, we used the CBCT on the Varian Edge linear accelerator to validate MRCAT Pelvis for a subset of the patient group,” he says. “Since this linac is equipped with iterative CBCT, the image quality is sufficient to recalculate the plan after each fraction [1].”
Mr. Bolard and Dr. Champion found good agreement between MRCAT-based and CT-based dose calculations, with a mean dose ratio of 1.007 (0.991-1.014).
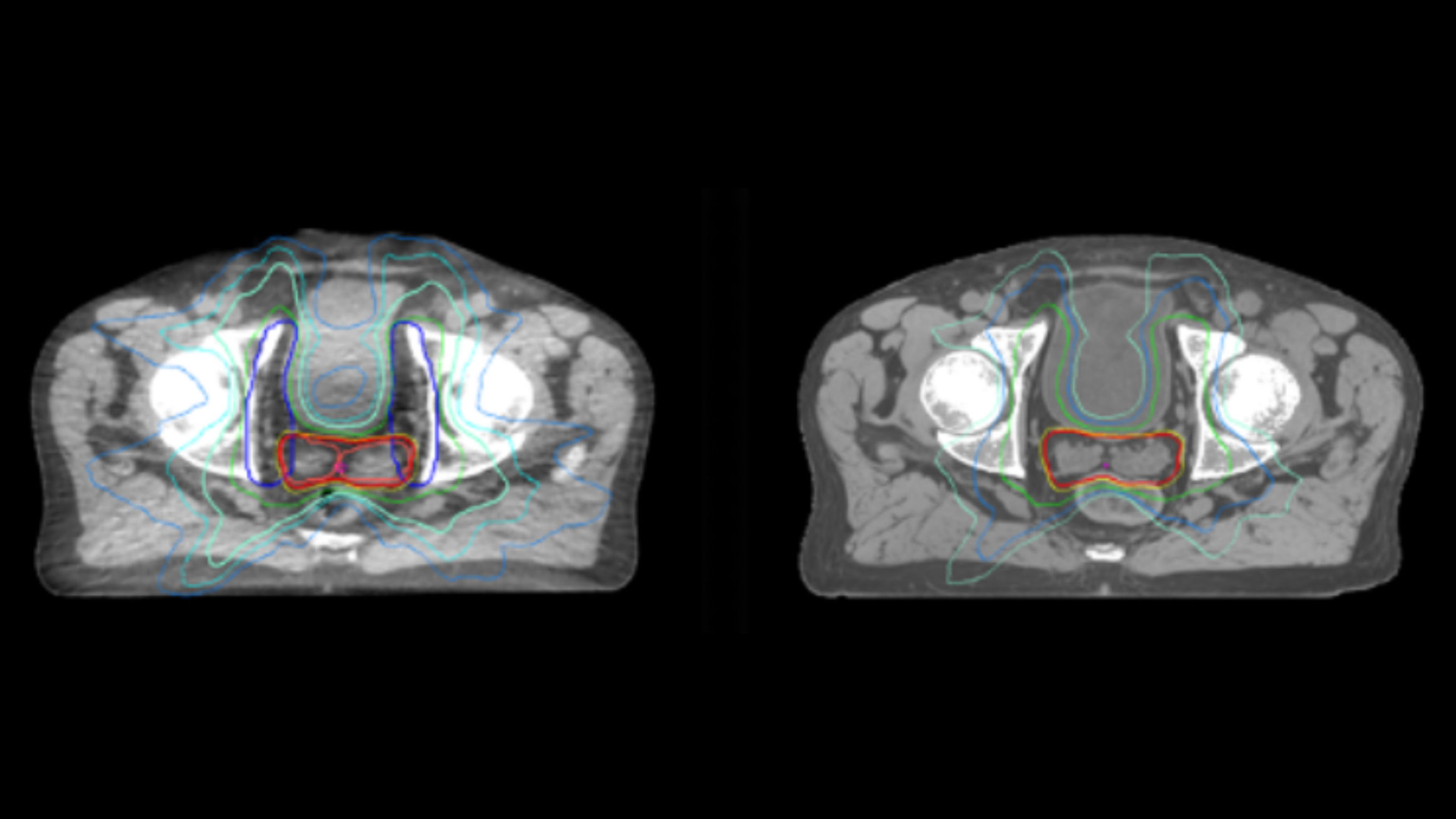
Dosimetric equivalence validation was performed on 43 patient cases by comparing MRCAT-based dose plans overlaid on CBCT image dataset and on the corresponding MRCAT image dataset. Mr. Bolard and Dr. Champion found good agreement between MRCAT-based and CT-based dose calculations, with a mean dose ratio of 1.007 (0.991-1.014). The 3D gamma score was greater than 95% (95.2-99.0%) for all plans checked. A poster on this work was accepted for presentation at ESTRO 2020 [4].
The erectile plexus and mesorectum are much better visualized on MRI than on CT. The same applies to the cranial limit of penile bulb, where we can more confidently spare this sensitive structure

The introduction of MR-only simulation for pelvic cancer radiotherapy planning has streamlined the workflow and increased confidence in target and OAR delineation, according to the La Tour team.
The simulation workflow is straightforward, with the RTT performing the positioning using the anterior coil support to prevent contact of the coil with the patient. No external laser positioning system is used. Instead, the La Tour team relies on the internal laser and a house-made ruler system for origin localization. Daily CBCT soft tissue matching against the MRCAT image set is performed, leading to a lean and satisfying workflow.
"We save more than an hour-and-half in plan preparation as compared to a workflow where we would register CT with diagnostic MR series that are not designed to RT needs," Mr. Bolard notes. “We also increase accuracy, since typical diagnostic sequences use large slice thicknesses and limited FOVs, which makes registration difficult to perform.”
We save more than an hour-and-a-half in plan preparation
The enhanced soft tissue visualization versus CT has made contouring much simpler, Dr. Champion adds. “MRI offers much better discrimination of the anatomical cleavage points, which improves contouring accuracy and reproducibility,” he says. “For example, the erectile plexus and mesorectum are much better visualized on MRI than on CT. The same applies to the cranial limit of penile bulb, where we can more confidently spare this sensitive structure, thus minimizing the risk of radiation-induced erectile dysfunction. And, although the rectal and bladder walls can be well-visualized on CT, MRI provides finer definition.”
In addition to allowing easier contouring, MR-only radiotherapy potentially improves the long-term results of specific toxicities of radiation therapy, Dr. Champion adds.
“Moreover, it has direct consequences on the margins we apply to the prostate clinical target volume (CTV),” he says. “Teams working exclusively on CT scans usually use isotropic margins of seven to five millimeters, except for the back where the margin is five to four millimeters. With MRI support, we are comfortable using four-millimeter isotropic margins.”
Hôpital de La Tour uses an implanted rectal spacer (SpaceOAR®, Boston Scientific) for patients receiving prostate radiotherapy to provide space between the rectum and prostate. 3D T2W TSE MRI provides excellent rectal spacer visualization and is used for OAR and target contouring. The dose plan is calculated on the MRCAT dataset.
Simulation imaging:
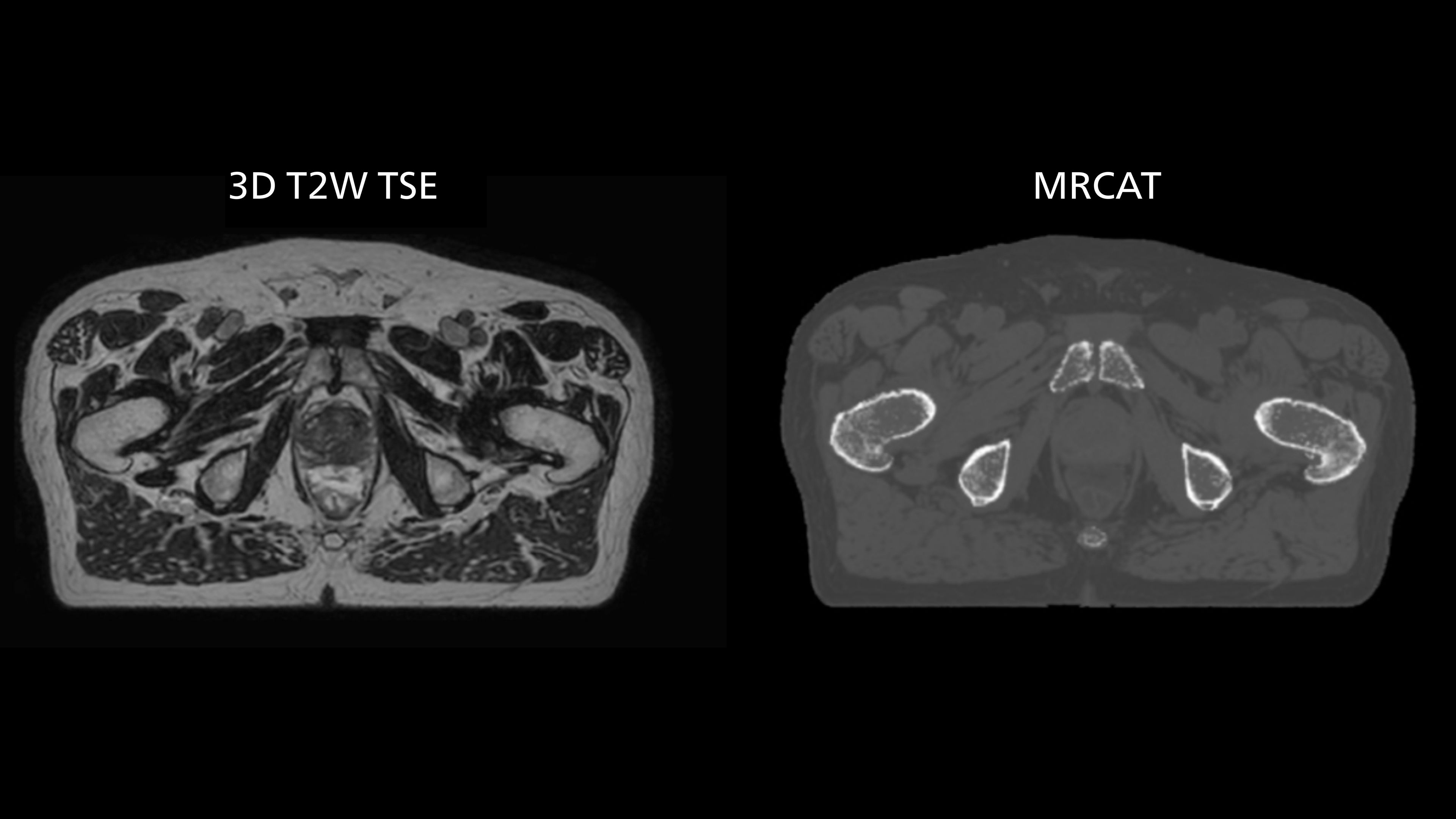
Transversal 3D T2W TSE with Compressed SENSE, acquired on Ingenia MR-RT 1.5T (left). On-console generated MRCAT (right).
MRCAT is primary image dataset for dose calculation (left). 3D T2W TSE MRI with 36 cm Field-of-View is used for delineation of prostate and organs at risk (right).
Speeding exams with Compressed SENSE
The Ingenia 1.5T MR-RT scanner is also equipped with Compressed SENSE, which helped the team to shorten scan times.
“Compressed SENSE accelerates our image acquisition by 20 to 40 percent to reduce the time needed per patient and therefore improves patient comfort and workflow efficiency with no change in image quality,” Dr. Breuneval says. “This benefits all our patients undergoing MR simulation. In particular for pelvic patients, – who must have an uncomfortably full bladder during their exam to improve visualization – this is a major benefit.”
Compressed SENSE improves patient comfort and workflow efficiency with no change in image quality.

MRCAT Pelvis is flexible, yet robust
Dr. Champion appreciates that MRCAT Pelvis also enables rectal cancer simulation in the prone position, allowing the digestive anatomy to be moved away from the treatment volume by projecting them forward.
“The irradiation volumes for a rectal cancer are essentially posterior and lateral, so good sparing of the digestive structures improves tolerance of the treatment,” he says. “Prone positioning can also be applied to anal cancer simulation. This position enables the gluteal muscles to be moved apart, which significantly reduces the toxicity associated with radiation concentrating in the folds.”
MRCAT Pelvis also allows an up to 36-centimeter FOV in the feet-head direction, permitting creation of treatment plans covering extended pelvic targets. “The large field-of-view is definitely useful and a must-have functionality,” Dr. Champion observes. “For several patients, we have treated the lymph nodes where the radiation fields are longer than 30 centimeters. In our practice, contouring of the pelvic lymph node areas is indicated in prostate cancers of intermediate or high risk. Rectal and anal canal cancer are also irradiated in the lymph node drainage areas. The cranial limit of this elective lymph node irradiation extends up to the aortic bifurcation, which often corresponds to the L4-L5 vertebral disc.”
Looking back on the last year of MRCAT Pelvis experience, Dr. Champion can point to several advantages for patients, staff and workflow efficiency.
“We have benefited not only from more precise tumor delineation and better OAR sparing, but also the elimination of the uncertainties of image fusion is particularly important,” he says. “It is also clearer and simpler for patients, who are now prescribed a single appointment to prepare for their treatment.”
“The logistical benefits are significant,” Dr. Champion adds. “MR-only radiotherapy avoids the need for an additional imaging examination and also reduces the costs associated with treatment planning. It’s also noteworthy that decreasing the number of examinations relieves the booking staff of these.”
We have benefited not only from more precise tumor delineation and better OAR sparing, but also the elimination of the uncertainties of image fusion is particularly important.
After having established MR-simulation as routine in their clinical practice, the team is committed to further expand their MR-only radiotherapy program to their brain cancer radiotherapy planning.
“MR-only simulation is a paradigm shift in radiotherapy planning. In the future I foresee it becoming progressively more widespread globally and feasible for more anatomical regions,” Dr. Champion says. “We at Hôpital de La Tour are proud to be pioneers in this field to provide the highest level of patient care.”
MRI boosts treatment quality and patient experience in radiotherapy
