
Expert perspective: quantifying liver fat with ultrasound
- Featuring
- March 17 2025
- 3 min read
Expert perspective: quantifying liver fat with ultrasound
This research report explores the expert perspective of Richard G. Barr, MD, PhD, FACR, FSRU, FAIUM on the use of ultrasound as a liver fat quantification tool. Dr. Barr is President, Radiology Consultants, Inc. (Youngstown, Ohio); Medical Director, Southwoods Imaging; and Editor In Chief, American Institute of Ultrasound in Medicine (AIUM).
At-a-glance:
- Ultrasound allows clinicians to detect liver disease early in its progression
- Elastography has proven useful in quantifying fibrosis and cirrhosis
- New ultrasound technique called attenuation imaging can detect and quantify liver fat in NAFLD (Non-alcoholic fatty liver disease)
- The widespread use of attenuation imaging could be very useful in screening for advanced chronic liver disease

Linked strongly with obesity, non-alcoholic fatty liver disease (NAFLD) is a significant health problem worldwide, affecting as many as one billion people. [1] Current reference standards for diagnosing and measuring NAFLD – liver biopsy and MRI – are impractical for various reasons. The emerging technique of ultrasound attenuation imaging could be helpful in screening for NAFLD. The method is non-invasive and can be done in less than three minutes with good technique. [2]
Ultrasound emerging as liver fat quantification (LFQ) tool
Continued developments in ultrasound technology are allowing clinicians to detect and stage liver disease earlier in its progression. [3] Ultrasound techniques such as elastography [4] have proven useful in quantifying fibrosis and cirrhosis, and a relatively new ultrasound technique called attenuation imaging has been developed to detect and quantify liver fat in NAFLD.
Who’s affected by NAFLD?
- Data from 1988 to 2008 show that NAFLD has doubled in the USA during that time period. [5]
- Characterized by accumulation of fat in ≥5% of hepatocytes in the absence of significant alcohol consumption (<30 g/ day for men and <20 g/day for women) or secondary causes of hepatic steatosis. [6]
- USA projections indicate a 21% increase in NALFD from 2015 to 2030, leading to a 33.5% overall prevalence by 2030. [7]
Attenuation imaging at Southwoods Imaging
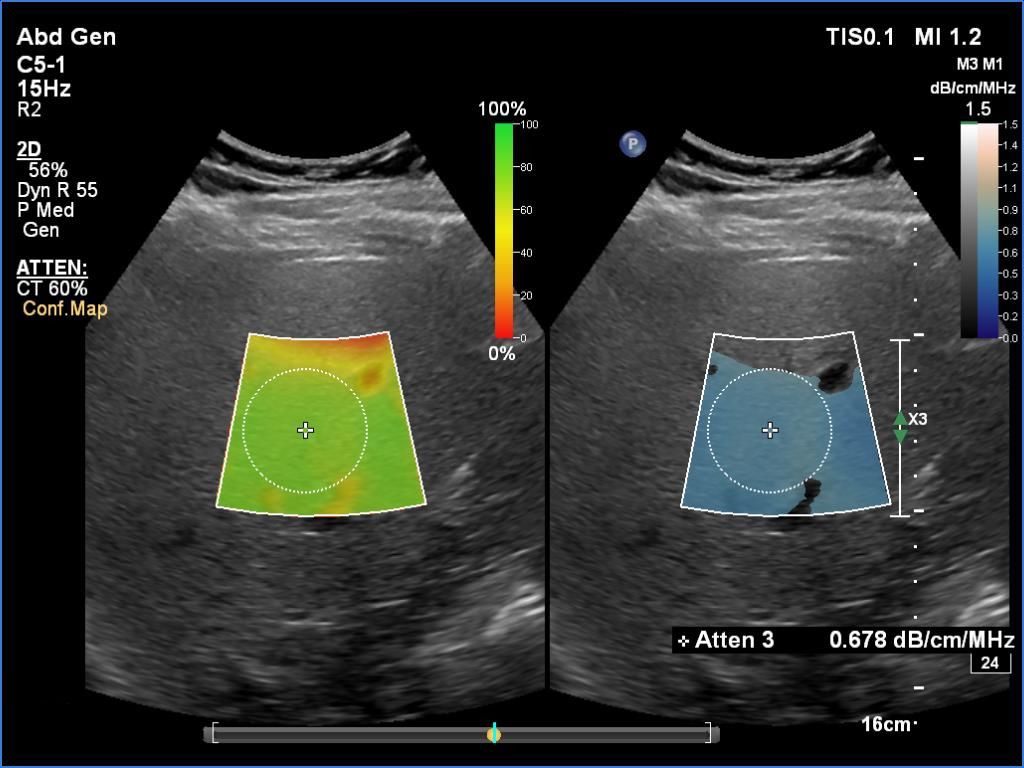
Attenuation imaging is based on the principle of ultrasound attenuation, the measure of how much sound is absorbed as it propagates through the liver parenchyma. It essentially calculates the attenuation coefficient (the rate of amplitude loss) as the pulse travels through tissue. The presence of fat in the hepatic tissue raises the attenuation and reduces the received signal amplitude more than comparable hepatic tissue without fat infiltration.
Dr. Barr has been performing attenuation imaging on patients whose doctors have requested diagnostic liver tests. Patients are typically referred to Southwoods Imaging to determine the cause of right upper quadrant pain and abnormal liver function tests. Dr. Barr says that in the past, he was only able to give a qualitative assessment of liver fat. “Now that there is a quantitative way of measuring liver fat, it will make it a lot easier for us to let the referring physician know where the patient is quantitatively on the NAFLD spectrum,” he says.
For some of these patients, referring physicians also request elastography to obtain a measure of liver stiffness. Both attenuation imaging and elastography can be done during the same ultrasound examination with the patient in the same position and using the same transducer.
“We need to intervene with these individuals before NAFLD turns into NASH [non-alcoholic steatohepatitis], because once that stage is reached, they could develop cirrhosis, hepatocellular carcinoma and/or liver failure,” he says.
With the combination of quantitative fat liver assessment via attenuation imaging and liver stiffness through elastography, the probability of NASH can be better assessed.

Richard G. Barr, MD, PhD, FACR, FSRU, FAIUM
Medical Director
Southwoods Imaging
Conclusions
Dr. Barr stresses that the goal in attenuation imaging is not necessarily to identify a cut-off value between mild and moderate steatosis, but to observe changes between successive scans.
In all, Dr. Barr’s center has used attenuation imaging on over 200 patients, including more than 100 patients who were part of a retrospective study [8] of chronic liver disease by multiparametric ultrasound, which encompassed attenuation imaging and shear wave imaging. The study concluded that the widespread use of attenuation imaging among the general population could be very useful in screening for advanced chronic liver disease.
“In our practice, almost 50% of the patients for whom we do a liver ultrasound have some degree of fatty infiltration of the liver,” says Dr. Barr. “With the combination of quantitative fat liver assessment via attenuation imaging and liver stiffness through elastography, the probability of NASH can be better assessed.”
Copy this URLto share this story with your professional network
Sign up for news and updates

Footnotes
- Loomba R, Sanyal AJ. The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol. 2013 Nov;10(11):686-90. doi: 10.1038/nrgastro.2013.171. Epub 2013 Sep 17. PMID: 24042449.
- Richard Barr, MD: Interview August 13, 2021
- Ferraioli G, Soares Monteiro LB. Ultrasound-based techniques for the diagnosis of liver steatosis. World J Gastroenterol. 2019;25(40):6053-6062. doi:10.3748/wjg.v25.i40.6053
- da Silva LCM, de Oliveira JT, Tochetto S, de Oliveira CPMS, Sigrist R, Chammas MC. Ultrasound elastography in patients with fatty liver disease. Radiol Bras. 2020;53(1):47-55. doi:10.1590/0100-3984.2019.0028
- Younossi ZM, Stepanova M, Afendy M, Fang Y, Younossi Y, Mir H, et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin Gastroenterol Hepatol. 2011;9:524–530.e1. doi: 10.1016/j.cgh.2011.03.020. [PubMed] [CrossRef] [Google Scholar]
- Puri P, Sanyal AJ. Nonalcoholic fatty liver disease: Definitions, risk factors, and workup. Clin Liver Dis (Hoboken) 2012;1:99–103. doi: 10.1002/cld.81. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Estes C, Razavi H, Loomba R, Younossi Z, Sanyal AJ. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018;67:123–133. doi: 10.1002/ hep.29466. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Aitharaju V, De Silvestri A, Barr RG. Assessment of chronic liver disease by multiparametric ultrasound: results from a private practice outpatient facility. Abdom Radiol (NY). 2021 Nov;46(11):5152-5161. doi: 10.1007/ s00261-021-03225-2. Epub 2021 Jul 25. PMID: 34304291.
Disclaimer
Results are specific to the institution where they were obtained and may not reflect the results achievable at other institutions. Results in other cases may vary.