New data in JAMA Cardiology found that >8 in 10 patients needing CIED infection treatment are not treated according to Class 1 guidelines (from a 100% Medicare sample). Yet, CIED lead extraction within 6 days of diagnosis is associated with a 42.8% lower risk of death [1].

Lack of proper CIED infection treatment is a significant public health problem
Cardiac implantable electronic device (CIED) infection occurs when an infection – either in the pocket or blood stream – has attached to the device or leads. Once an infection is in the blood stream, leads act as a highway to the heart and can spread the infection.
The risk of CIED infection is rising, and the longer a device is implanted, the higher risk patients are for developing a device infection [2]. If patients are not treated appropriately with prompt CIED lead extraction, there is significant mortality and associated costs [3]. Left untreated, device infections can lead to endocarditis and death [4].
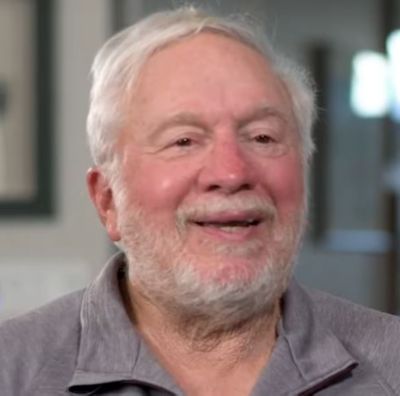
When Jerry, a pacemaker patient, experienced a sudden negative turn in his health, he and his wife Helane sought out answers. After working with multiple doctors and trying different treatments, it was finally determined Jerry had an infection of his heart device. Watch Jerry's incredible story and learn more about CIED infection treatment.

By removing the pacemaker, I’ve been able to get on with my life and be more optimistic about tomorrow, and I can live again.
There are two types of CIED infection: pocket infection or systemic infection.
Pocket infection
A pocket infection begins in the pocket where the generator is implanted and attaches to the leads. A pocket infection can occur at the time of implantation or any time thereafter. The risk of infection increases every time the pocket is manipulated [5]. Symptoms of pocket infection may include [6]:
Systemic infection
Systemic infection may develop elsewhere in the body - such as from a cut or wound that becomes infected and enters the bloodstream, eventually working its way to infect the leads and subsequently, the heart. Symptoms of systemic infections may be more elusive and general in nature, such as:
Identifying the source of a CIED infection can be difficult. However, with the incidence of infection on the rise [5], it is important to investigate the device if an infection is present. A 100% Medicare sample study confirms a gap in guideline driven knowledge and care for CIED infections [1]. Only 29% of cardiologists are familiar with CIED infection guidelines and 30% of physicians have protocols for managing CIED infection at their institution [9].
Over a 10-year period there has been a 320% increase in CIED infection rates and over 31,000 of US device patients are diagnosed with an infection each year [2,5,8]. CIED infection can be fatal if not treated appropriately and currently more than 80% of CIED infection patients fall into this category [1]. CIED infection is a Class I indication for complete system extraction [12].
320% increase in CIED infection rates over a 10-year period [5] | >31,000 US device patients diagnosed with an infection each year [2,8] | >8 in 10 Patients not treated appropriately [1] (from a 100% Medicare sample) |
With early diagnosis and appropriate treatment, cardiac device infections can be cured [1]. Lead extraction has a 97.7% clinical success rate and a 99.72% procedural safety rate [10,11], which is why all major cardiac society guidelines recommend complete system removal of hardware and leads when an infection is present [12].
97.7% Clinical success rate [10,11] | 99.72% Procedural safety rate [10,11] |
In many cases, infections are caused by antibiotic-resistant staphylococcal bacteria that live in colonies called biofilm. The biofilm forms a thick coating around the device or leads that is nearly impossible to cure with antibiotic treatment alone [13].
Infection relapse occurs in 50% to 100% of cases with partial removal or antibiotic treatment alone, compared to 0% to 4.2% relapse with complete system removal [7,14-17]. There is also a seven-fold increase in 30-day mortality for antibiotic treatment with device removal and a 42.9% lower risk of death when a patient’s leads are extracted within six days of CIED infection diagnosis [1,7].
7x increase in mortality 7-fold increase in 30-day mortality for antibiotic treatment without device removal [7] | 42.9% lower risk of death When leads are extracted within 6 days of CIED infection diagnosis [1] |
New data: Only 50% of cardiologists recommend guideline-driven care for CIED infections [9]