Building the silent ICU of the future: Philips to demonstrate a collaborative approach to interoperability at #HIMSS24
Health Tech manufacturers collaborate with SDC-enabled technology to create a more peaceful healing environment for patients and streamlined workflow for clinicians
Mar 07, 2024 | 4 minute read
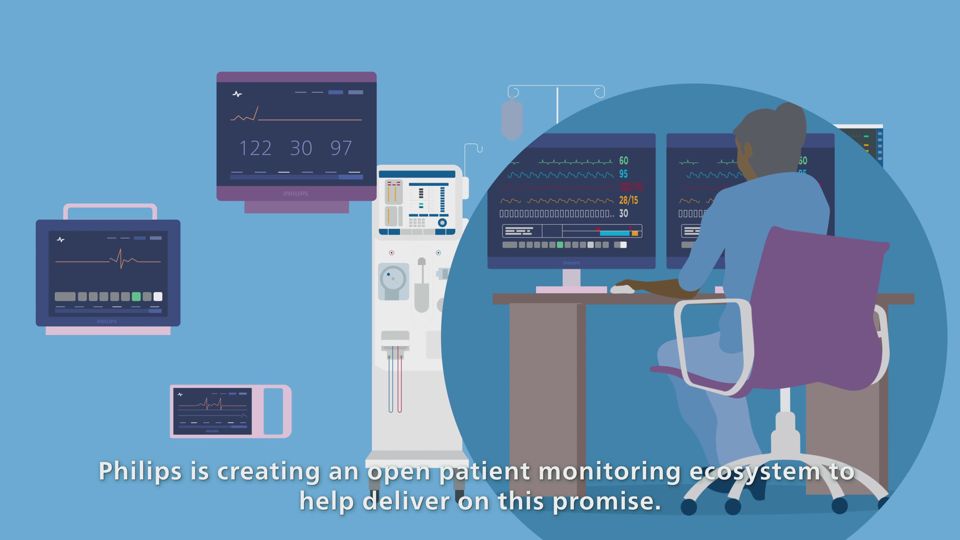
Today’s care providers are often burdened by the complexity of having to interpret siloed data from a variety of different screens, devices, and electronic medical records (EMRs) to determine the most effective treatment solutions for their patients. Only when viewed collectively can this information offer a comprehensive view of a patient's condition and help guide timely clinical interventions.

First developed to bring flexibility and interoperability to application development on the internet, service-oriented architectures (SOA) now hold promise for many industries, including healthcare. The average intensive care patient is estimated to produce over 1,200 data points every day. [1] With many vendors in the market collecting patient data, a lack of interoperability among medical devices could lead to preventable clinical errors and workflow inefficiencies. While technology holds the power to transform healthcare into an efficient and seamless experience for patients and care providers alike, its full promise can only be realized when vendors work together.
This thinking became a catalyst for the IEEE 11073 service-oriented device connectivity (SDC) family of standards, born from the SOA model. The new SDC standards support open communication between health technology providers and can replace proprietary networks with a common language for communication between devices. By enabling the interoperability and exchange of data, patient information can be shared bi-directionally and securely in near real-time. SDC-enabled medical devices can radically change clinicians’ experiences, allowing them to see and act upon data derived from integrated acute care technologies – such as patient monitors, sensors, ventilators, and infusion pumps – regardless of manufacturer.
Philips is joining forces with like-minded medical device manufacturers to further define and deploy SDC standards across the industry. Many of these companies will come together at HIMSS 2024 in Orlando, Florida to demonstrate real-world applications and showcase the benefits of collaborative, cross-vendor interoperability. Once the SDC protocol is released and backend capabilities are more broadly adopted, SDC will help hospitals to standardize device communication and provide consistent access to previously siloed data, enhance cybersecurity with end-to-end encryption, and enable a centrally managed, common infrastructure that features vendor-neutral, remote device management.
“Service-oriented architecture presents the health technology industry with an opportunity to collaborate to achieve a common goal,” says Christoph Pedain, Business Leader, Hospital Patient Monitoring at Philips. “We’re moving away from proprietary communication protocols and closed ecosystems, advocating for vendors to prioritize SDC-readiness and help create a truly open and interoperable healing environment for patients and a more streamlined workflow for our customers.”

New capabilities in action: the Silent ICU
In intensive care environments, patients are surrounded by numerous devices, each serving vital functions but also emitting alarms that demand attention. These alarms can disrupt the patient's environment, hinder sleep, potentially complicate recovery, and prolong healing.
Potential SDC-enabled care environments, such as the Silent ICU, will utilize smart technologies to create a more peaceful healing space. Philips, along with other health technology companies, will showcase this concept at HIMSS. Philips intends to collaborate with hospitals and health tech firms to enable clinicians to manage alarms remotely, enhancing patient care. Existing Philips technology allows clinicians to silence alarms from Philips monitors and distribute alarms for third-party devices. While this can help make patient rooms quieter, clinicians must enter a patient’s room to act on an alarm, which could unnecessarily disrupt the patient’s recovery. In a Silent ICU, SDC-enabled devices with bi-directional capabilities and an open ecosystem will change this dynamic. Clinicians will have access to patient information remotely, from a nursing station, central monitoring unit, or mobile device, and can accept and adjust alarms from anywhere, potentially improving patient recovery experiences as all SDC-enabled device alarms can be muted in the patient room.

Philips has actively taken steps to provide a more open ecosystem to our customers, most recently seen in the acquisition and integration of Philips Capsule Medical Device Information Platform into the Philips Patient Information Center (PIC iX) and mobility solutions. SDC allows us to expand upon data acquisition to provide a more modernized, bi-directional integration foundation to improve workflows and build advanced clinical use cases. An SDC-enabled care environment allows us to expand our ecosystem beyond hospital walls to include medical technology manufacturers across the healthcare industry.
Philips will offer a first glimpse of SDC enablement in action in the Silent Patient Room at the HIMSS Interoperability Showcase from Tuesday, March 12 through Thursday, March 14. Demonstrations will take place every 90 minutes during show hours, with a special presentation on the future of Philips’ open ecosystem strategy on March 13 at 11:15 a.m. EDT, led by Philips’ Christoph Pedain. To learn more about Philips emerging SDC-enabled capabilities or its portfolio of patient monitoring solutions, visit booth #2041 at HIMSS or Philips.com/SDC.
Sources [1] Manor-Shulman O, Beyene J, Frndova H, Parshuram CS. Quantifying the volume of documented clinical information in critical illness. J Crit Care. 2008 Jun;23(2):245–50








