Don’t lose good days to bad nights
Find out if you are at risk for sleep apnea

Find out if you have symptoms of sleep apnea

Don’t lose good days to bad nights
Find out if you are at risk for
sleep apnea
Find out if you have symptoms of sleep apnea
What is sleep apnea?
Obstructive sleep apnea (OSA) is a common sleep disorder characterized by repeated interruptions in breathing throughout the sleep cycle. These interruptions, called apneas, are caused by the collapse of soft tissue in the airway, which prevents oxygen from reaching the lungs.
Obstructive sleep apnea
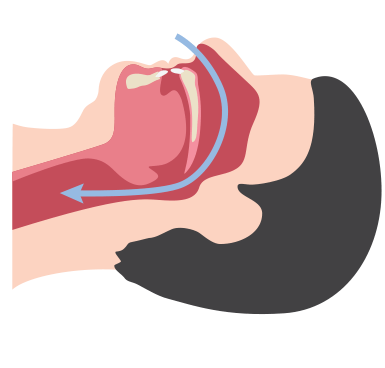
Non-obstructed airway
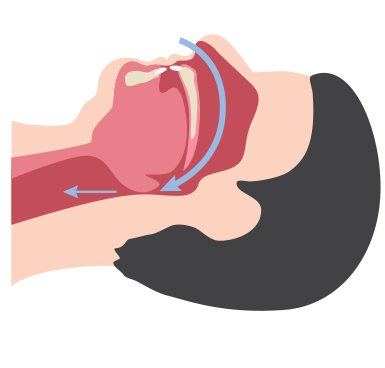
Obstructed airway
You’re not alone
Obstructive sleep apnea may not only be affecting you, but also could be affecting your loved ones. Learn how sleep apnea can influence people just like you.
Car incident
Jesús relationship
Cheryl's children
About 10% of the adult population in the world suffers from sleep apnea, and about 90% of them have not been diagnosed.1 In the US, 7% of men are living with sleep apnea. 5% of women are living with sleep apnea. According to the American Academy of Sleep Medicine Frost and Sullivan report from 2016, approximately 12% suffer from obstructive sleep apnea, at least 29.4 million adults in the U.S. - 80% of which go undiagnosed. That’s significant because sleep apnea is a serious condition. Sleep apnea disrupts the sleep cycle and can dramatically impact energy, mental performance and long-term health. In some cases, if left untreated, sleep apnea can be fatal.
It can be hard to take the first steps into finding out if you have sleep apnea.
We are here to help.
Sleep apnea symptoms and risks
Untreated sleep apnea is associated with a number of health risks, so it’s important to consult a sleep specialist if you have these signs and symptoms.

Nighttime symptoms

Daytime symptoms
*Mayo Clinic, “Sleep Apnea Complications,” August 2015. http://www.mayoclinic.org/diseases-conditions/sleep-apnea/basics/complications/con-20020286
Additional resources

Get the most out of your treatment options in our You have sleep apnea, now what? brochure.
What are the risks of untreated sleep apnea?
Sleep apnea can have serious short- and long-term health risks if left untreated, including:
How do I get diagnosed?
If you think you have sleep apnea, it’s important to find out for sure so that you can begin treatment and start enjoying the benefits of better sleep and a healthier life.

Take the symptoms quiz to determine if you are having symptoms of sleep apnea. Print out your results to take to your doctor.

Discuss your sleep apnea risk test results with your primary care doctor, who will likely help you schedule a sleep study.

Look into sleep testing options, including asking your doctor whether your health condition allows for in-home sleep testing.

Once you receive your diagnosis from your doctor they can tell you which OSA solutions are right for you.
Benefits of getting tested

Myth: I don’t think I will be comfortable sleeping in a sleep lab.

Fact: Though many people have this fear, most are able to fall asleep in the sleep lab.
By Teofilo Lee-Chiong, MD, chief medical liaison, Philips Healthcare Solutions
Sleep studies 101
Getting diagnosed: personal experiences Hear from people who took the leap and met the challenges involved in getting diagnosed. Watch now
What is AHI?
What determines if you have positional obstructive sleep apnea? Positional obstructive sleep apnea is defined as having two times or greater the AHI when sleeping on your back as opposed to when you are on your side.5
The Apnea Hypopnea Index (AHI) is the most important number on your sleep apnea test. It measures the number of times you have an apnea (when you stop breathing for a short time) or hypopnea (when you partially stop breathing for a short time) while you’re asleep.
Understanding your sleep study results
Your doctor ordered an overnight sleep study (also called a polysomnogram or PSG) either in a sleep center or your home, to determine if you have sleep apnea. After you complete the sleep study, your doctor will give you the results and discuss what to do next. You may be given a copy of your sleep study report. The report is going to include information on how you slept such as: how long you slept, your Apnea Hypopnea Index (AHI) or how many times you stopped or partially stopped breathing and if your oxygen is saturated. The defining numbers of OSA are based upon your AHI. Alternatively, if your numbers fluctuate between sleeping on your side versus on your back, you may have Positional Sleep Apnea (POSA), defined as AHIsupine ≥ 2 x AHInon-supine.2

You have sleep apnea, now what?
AHI <5 | Normal3 |
AHI 5-15 | Mild3 |
AHI 15-30 | Moderate3 |
AHI >30 | Severe3 |
Health insurance coverage for:
Sleep Studies4
Medicare, as well as most insurance companies, will provide payment for a medically-indicated sleep study. While sleep studies have traditionally been performed in a sleep lab during an overnight stay, Medicare and many other insurance companies now also pay for in-home sleep studies used to diagnose Obstructive Sleep Apnea (OSA). It is important to contact your insurance company to determine if they will be paying for an in-lab or in-home sleep study and to understand any deductible or co-payment amounts that will be your responsibility to pay.
Sleep Therapy5
Medicare and most other insurance companies will pay for a CPAP or bi-level device and related accessories and supplies, provided that specific coverage criteria are met. Coverage criteria is documented by, but is not limited to, the following: Your insurance company and your durable medical equipment (DME) supplier will be able to assist you in understanding what is covered, what documentation is required, and any financial responsibility you may have, such as deductibles or co-payments
Frequently asked questions
- What is obstructive sleep apnea?
-
Obstructive sleep apnea is a condition in which a person stops breathing repeatedly through the night. Breathing stops because the throat or “airway” collapses and prevents air from getting into the lungs. Sleep patterns are disrupted, resulting in excessive sleepiness or fatigue during the day.
- How many people in the United States have sleep apnea?
-
According to the American Academy of Sleep Medicine Frost and Sullivan report from 2016, approximately 12% suffer from obstructive sleep apnea, at least 29.4 million adults in the U.S. - 80% of which go undiagnosed.
- What causes the airway to close during sleep?
-
- Extra tissue in the back of the airway, such as large tonsils
- Decrease in the tone of the muscles that hold the airway open
- The tongue falling back and closing off the airway
- What should you do if you think you may have sleep apnea?
-
Evaluation by a doctor specializing in sleep disorders is recommended. Have a sleep study done. A sleep study can provide the doctor with information about how you sleep and breathe. This information will help the doctor to determine your diagnosis and treatment options.
- What are the risks of untreated sleep apnea?
-
Sleep apnea can have serious short- and long-term health risks if left untreated, including:
- High blood pressure
- Irregular heartbeat
- Heart disease / heart attack
- Stroke
- Type 2 diabetes
- Driving- and work-related accidents
- What is the treatment for sleep apnea?
-
Most commonly, positive airway pressure (PAP) therapy is the treatment. It is noninvasive and can help with symptoms when used as prescribed. Less commonly, surgery or oral appliances are used, which may be effective in certain cases. Any treatment plan should include weight loss if needed, exercise and avoiding alcohol, sedatives and hypnotics.
- How does PAP or CPAP therapy work?
-
CPAP (Continuous Positive Airway Pressure) provides a gentle flow of positive-pressure air through a facial mask to keep the airway open during sleep. As a result:
- Breathing becomes regular during sleep
- Snoring stops
- Restful sleep is restored
- Quality of life is improved
- Risk for high blood pressure, heart disease, heart attack, stroke and motor vehicle and work accidents are reduced
- What are the nighttime symptoms of sleep apnea?
-
- Loud or disruptive snoring
- Witnessed pauses in breathing
- Choking or gasping for air during sleep
- Restless sleep
- Frequent visits to the bathroom
- What are the daytime symptoms of sleep apnea?
-
- Early morning headaches
- Excessive daytime fatigue
- Poor concentration
- Depression or irritability
- Falling asleep during routine activities
- What can put you at increased risk for sleep apnea?
-
- Overweight/obesity
- A large neck or tongue
- Extra tissue or crowding in the airway
- What does an apnea episode look like?
- What are the benefits of regular usage of PAP therapy?
-
Most PAP users who remain committed to treatment enjoy:
- Increased energy and attentiveness
- Fewer morning headaches
- Reduced irritability
- Improved memory
- Increased ability to exercise
- Lower blood pressure
- Decreased risk of strokes and heart attacks
- Increased effectiveness at home and at work
- Improved overall quality of life
Need product support?
Are you a sleep professional?
Did you have a good experience with a Philips product? Help others like you.
References 1 Young T, et al. Epidemiology of obstructive sleep apnea: a population health perspective. AJRCCM 2002;165:1217-1239. For informational purposes only, not to replace physician's directions. 2 Cartright criteria, Effect of Sleep Position on Sleep Apnea Severity, R. Cartwright, 1984. (https://www.ncbi.nlm.nih.gov/pubmed/6740055) 3 What does "AHI" represent? Sleephealth.org. American Sleep Apnea Association. (https://www.sleephealth.org/ufaqs/what-is-ahi-represent) 4 Mador. MJ. et al. Prevalence of positional sleep apnea in patients undergoing polysomnography. Chest 2005 Oct. 128(4) 2130-7 5 Cartwright criteria, Effect of Sleep Position on Sleep Apnea Severity, R. Cartwright, 1984.