Don't have time to read the guide now? Download a PDF
Introduction
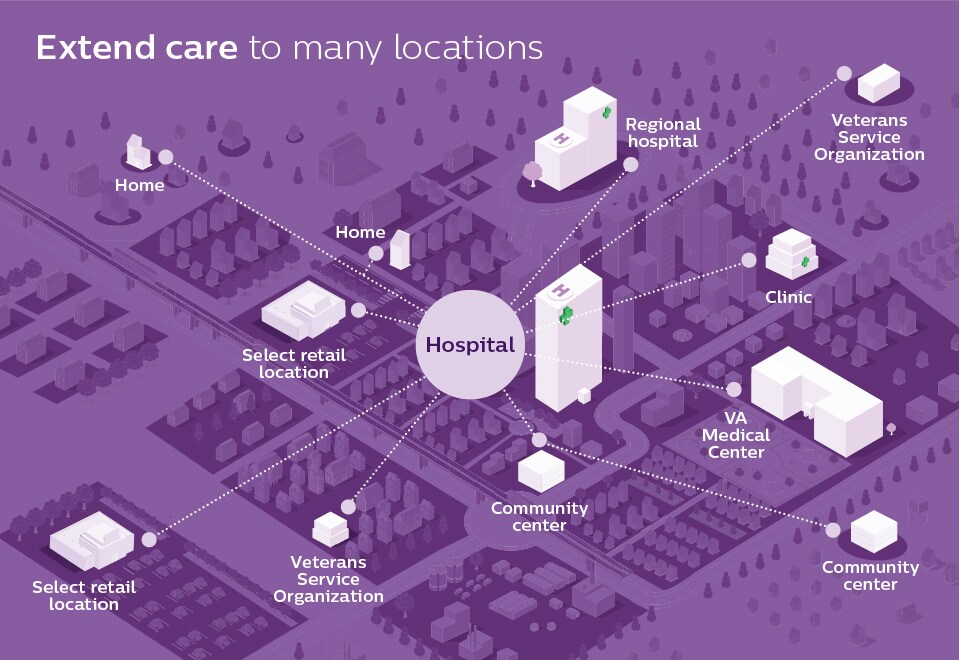
A crucial opportunity to extend care between and beyond hospitals and into the home This is a critical moment in our nation’s history, and we must respond to the urgency of the moment by building a stronger healthcare system that extends care delivery to everyone – no matter where they live and work – helping them receive care in a secure and flexible way that fits their day-to-day lives. We have an opportunity to reach our nation’s patient population including active-duty military members and veterans in communities near and far, provide greater care for American Indians and Native Alaskans and further support those served by Medicaid, Medicare and our federal government’s other vital healthcare programs. We believe a stronger healthcare system begins with a healthier population. To help people stay healthy, prevent illness and receive care when and where they need it, our hospitals – the foundation of our healthcare system – must extend care beyond their walls. By extending care to communities, workplaces and homes, hospitals can become more resilient and patient-centric, helping patients take care of their health in places that are convenient and comfortable for them. Historically, extending that care meant accepting trade-offs in precision and accuracy, but today’s cutting-edge solutions allow health systems to deliver hospital-quality care to the home and other settings. In doing so, we change the role of the hospital from the central event in a patient’s healthcare journey to a peripheral event, or an event we successfully help to avoid by providing quality care all along the way. The transition to prioritizing outpatient care has been underway for some time, but the pandemic – and the national response to it embodied in the CARES Act – have given new urgency to the shift toward extended care delivery. It is a transformative shift powered in part by telehealth and virtual care, AI-enabled decision-making tools and interconnected devices that seamlessly track patients along their journey.
Reaching patients no matter where they are Extending care benefits patients, especially those in rural areas without easy access to a hospital, those with chronic conditions who need ongoing monitoring and coordinated care and those with disabilities for whom a trip to the hospital or the rehabilitation facility may be unnecessary. In some areas, emergency room visits have decreased by 42% year over year, in large part due to concerns about COVID-19.1 But avoiding the hospital does not have to mean avoiding care. Telehealth can proactively monitor and step in to provide timely intervention for those at risk and can do so in a high-quality, cost-effective way, which can result in substantial cost savings (to patients served by Medicare or Medicaid, for example).
“Whether in the hospital, doctor’s office or home, we are connecting patients to their medical team, frontline caregivers to each other, isolated patients to their family and friends, and healthcare workers in all aspects of the business to each other and their work.” —Lisa S. Stump, Senior Vice President and CIO, Yale New Haven Health System and Yale School of Medicine
Supporting critical care missions Extending care to additional settings extends the capacity of caregivers, too. Health systems often need to address staff shortages and to align their staffing to better meet the needs of the patients they serve. Even before COVID-19, fewer than 15% of ICUs were able to provide care from an intensivist2 – and almost half of critical care physicians and nurses reported burnout.3 Extending care increases efficiencies and leads to better patient and caregiver experiences. It also helps control costs so resources can be put to other uses in support of health systems and the important missions of the Department of Veterans Affairs (VA), Department of Defense, Indian Health Service, Department of Health and Human Services and other essential government agencies. In this guide to extended care delivery, we suggest ways you can transform your health system, positioning you to provide the care your patients deserve and to support care providers in their valuable work.
Estimated reading time: 15 minutes
Share on social media
Two strategies for extending care
To close the capacity and capabilities gap, health systems will need to:
Two strategies for extending care
To close the capacity and capabilities gap, health systems will need to:
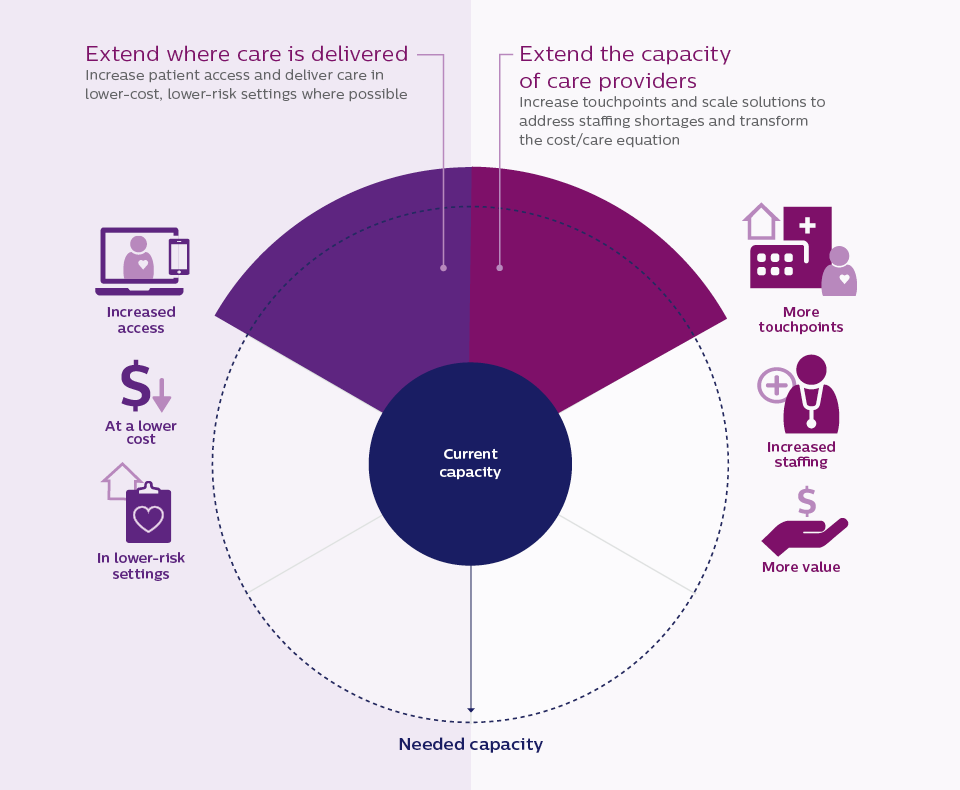
Health systems that adopt strategies to extend care delivery will get closest to achieving healthcare’s quadruple aim. At Philips, we are proud to provide the latest advancements in innovative and connected solutions to offer greater choices for how, when and where patients receive care.
Extend where care is delivered for a stronger health system
A stronger, more resilient healthcare system means continuing to move care beyond the hospital’s walls – to clinical offices, virtual care sites and patient homes – and augmenting that care with powerful, proactive artificial intelligence (AI) that complements the expertise of care providers.
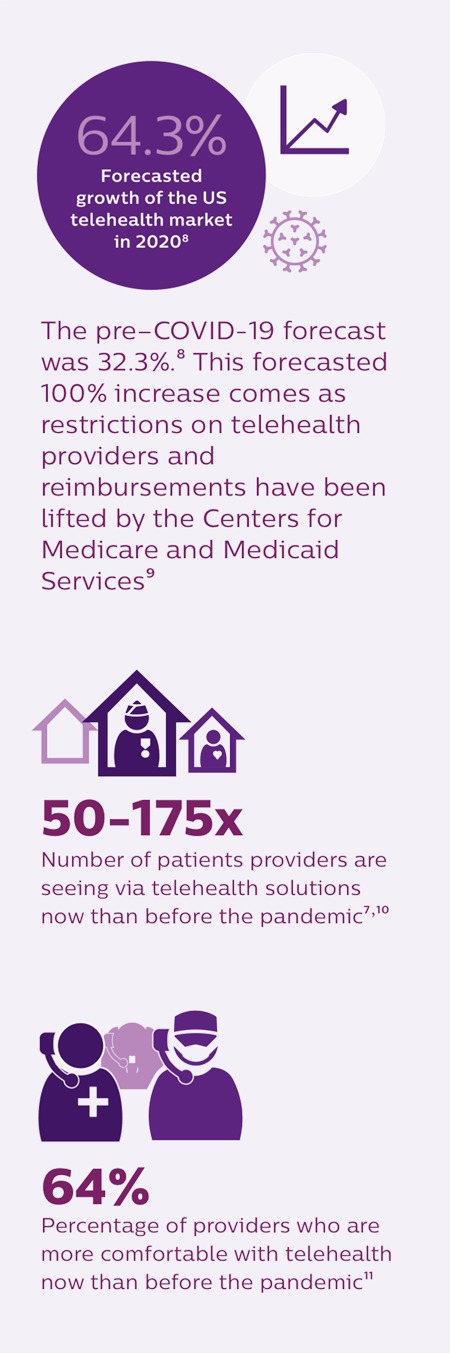
Untethering the patient to provide anywhere care Currently, many health systems struggle to serve aging, chronic and rural patients who may not have convenient access to hospitals. For example, 5 million veterans lived in areas designated as rural by the US Census Bureau during the 2011-2015 period,4 and as that population continues to age, the prevalence of chronic conditions like hypertension and diabetes is projected to rise by 12% and 8%, respectively.5 Difficulty in accessing care is exacerbated during pandemics, when reduced rates of admission for heart attacks, strokes and other emergencies suggest that patients are avoiding necessary care out of a fear of going to the hospital.6 By making care flexible and untethering patients from a centralized location and striving to provide care nearly anywhere, we can improve the continuity of care a health system provides. Care can be delivered in lower-cost and lower-risk settings and health systems can improve the consistency of care, focus on preventative care to keep patients healthier outside the hospital and, in the event patients must move between care settings, ensure that they are better served throughout their journey. The demand for extended care is expected to keep growing, driven by concerns about COVID-19, an aging population and a rise in chronic conditions that are rapidly transforming preferences for how and where care should be delivered. Bringing care to the home Virtual or telehealth visits can solve many of these challenges, and its use has massively accelerated in the wake of COVID-19. Consumer adoption in the US has skyrocketed from 11% of consumers in 2019 to 46% today.7 Telehealth solutions extend care to the home, allowing for remote screening and triage and helping to proactively manage patients in lower-cost settings. Additionally, this technology conserves equipment and hospital space for patients who need it, limiting the risk of exposure for hospital-based care teams, limiting potential patient exposure by allowing them to receive care from the safety of their home and reducing the overall cost of care, particularly for chronic populations – in some cases, improving costs by 2% to 3%.7 Recently, the VA and Philips joined forces to expand the VA’s tele-critical care program, an up to $100 million investment that can have a tremendous impact on improving veterans’ health.12 Care can also be extended with patient management solutions that guide, track and triage patients through multiple digital channels. Automated text messages and emails help patients get to their appointments, guide patients in their pre- and postoperative care and provide additional health information. These technologies can improve patient outcomes for everything from device-assisted sleep therapy to the management of chronic conditions. Providing nearby access Extending care means helping people manage their health and their schedule by connecting them with care providers in local settings. For patients who don’t have connectivity at home, virtual care sites are a convenient option and can be useful when the healthcare environment is disrupted, as it was because of COVID-19. Equipped with biosensors to monitor vitals, these solutions in select retail or community-based locations, and Veterans of Foreign Wars and American Legion posts dramatically increase healthcare access for millions of veterans in rural communities who otherwise face challenges accessing the nonacute care they need. In 2018, virtual care resulted in over 1 million telehealth visits at the VA, a record for the agency.13 Moving toward proactive care Through the use of AI, we can move beyond the current model of reactive sick care toward proactive care. At every step in people’s lives – from cradle to old age – AI-powered applications and health services can inform and support healthy living with personalized coaching and advice, guiding patients and care providers in the prevention and treatment of disease. These AI capabilities will supplement – not replace – care providers in a variety of care settings, helping to improve health outcomes. Some AI advances are highly useful right now (using predictive analytics to predict when an individual patient needs a particular intervention, for example). Using AI to get better health outcomes at the population level is certainly a worthwhile goal, but it will take more time to achieve.
Extend the capacity of care providers
Health systems often face staff shortages and must align staffing to better meet the needs of patients and communities. But currently, hospitals struggle with the reduced availability of expert clinicians. Night shifts can be the most challenging, as small teams of nurses and on-call doctors are spread thin, caring for entire floors of patients. Thus, standardization in many areas of care can suffer. Because of the limited number of intensivists and the cost to attract and retain them, many hospitals find it challenging to adequately staff their intensive care units 24/7. This problem is growing, as the supply of intensivists is projected to meet only 22% of the demand in 2020.14 Currently, just 47% of hospitals surveyed have the recommended intensivist coverage.15 By scaling how and where staff deliver care, health systems can enable better patient outcomes and transform the cost/care equation. This is important for rural communities and enterprise-wide settings, such as our multilocation military settings, where virtual health programs enable service members, their families and retirees to receive care anywhere, anytime – deployed in a battlefield, a field hospital, in a traditional military hospital or at their home.
Reinforcing care providers on the front lines Remote patient monitoring is one powerful way to reinforce busy care providers, aligning staff to care volumes and shifting patient monitoring and management to remote locations even halfway across the world where there is 24/7 support. This round-the-clock, remote surveillance by skilled professionals – and the decision-making algorithms that assist them – provides early warnings for proactive care and continuous programmatic improvement. Clinical command centers can also play an essential role in preventing and managing through a crisis, such as the pandemic. The University of Kentucky UK Healthcare System did exactly that. Working with Philips, they powered the state’s only tele-ICU clinical command center, enabling intensivists and critical care nurses to remotely manage ICU patients. This allowed their teams to prevent crises rather than merely respond to them.16 Patients requiring respiratory care benefit from remote monitoring. Ventilators connect with patient monitoring systems, identify significant deviations in patients’ vital signs and automatically verify the accuracy of the trend before notifying caregivers. This care can occur bedside with advanced monitors that can be viewed remotely. With these active displays, health systems can, among other things, create isolation areas that can be controlled from anywhere – a valuable asset when caring for patients with contagions. Telehealth solutions can help hospitals reduce patient transfers to other hospitals, reducing the burden on caregivers. A study from the VA tracked 553,523 patients admitted to 306 VA hospital ICUs from October 2009 through September 2015. During this period, the VA implemented tele-ICU at 52 ICUs in 23 facilities in 9 states aiming to provide remote access to comprehensive acute care expertise for smaller community and regional ICUs in its health system. The study showed that the use of tele-ICU allowed local ICUs to treat more critically ill patients on-site and reduce hospital transfers.17
Don't have time to read the guide now? Download a PDF
Shifting chronic care management from hospital to home Shifting care management for patients with chronic conditions from hospital to home may alleviate workload. By supporting chronically ill patients with connected devices, remote monitoring and customized clinical pathways to detect deterioration, care providers can intervene earlier, reduce costs and reduce readmissions. This can keep chronic oncology, cardiology and pulmonary patients out of the hospital during subsequent phases of treatment. All too often, patients with chronic conditions are not well managed. A study found that up to 71% of moderate-to-severe COPD patients from a Medicare population did not receive maintenance pharmacotherapy.19 Not surprisingly, patients whose COPD is unstable (frequent or severe exacerbations, faster decline in pulmonary function) can be more challenging and costly to manage, and they often end up back in the hospital.20 Philips Integrated COPD Care Initiative can help better manage the care of patients with COPD. In fact, this initiative resulted in an 80% reduction in acute 30-day readmissions and a >70% reduction in total all-cause acute care events by initiative end – driving a savings to the hospital of $1.3 million and $4.4 million, respectively.21 For veterans, or the elderly, who have an increased prevalence of COPD, these types of connected solutions can be a lifeline. 22-23 Remote care management is beneficial to health systems during pandemics, when staff is shorthanded and reintroducing patients with comorbidities into a hospital could worsen health outcomes. From a centralized and remote vantage point, care providers can triage patients by using automated acuity, guideline-based scores and predictive analytics. Care providers can even connect with patients using two-way live video, providing insight into patients’ living environments for more accurate assessment. More than 22 million Americans and 18% or more than 1 million veterans have obstructive sleep apnea. While these veterans need treatment, a recent assessment concluded that most VA sleep programs are understaffed and have lengthy wait times for appointments. Philips structured a patient adherence management solution to help patients stay with therapy. This solution utilizes telemonitoring of therapy device adherence data and a call center with sleep coaches and respiratory therapists. PAP adherence at 3 months improved by 25% using cloud-based sleep coaches versus standard care.24 Advising colleagues from afar When care providers need expertise for a patient case, or an extra set of eyes, remote peer-to-peer consultation solutions can bring real time expertise from off-site locations and distribute workloads among care providers. Across a variety of specialties, colleagues are remotely supporting each other, bringing expertise where and when it’s needed. Tele-radiology, virtual tumor boards, tele-ultrasound and remote emergency care collaboration help healthcare providers consult with each other for improved patient care. Remote peer-to-peer consultations can hasten diagnoses when EMS personnel or care teams in the battlefield need to make quick decisions. In these situations, the on-site care worker needs to capture large amounts of rapidly changing data, like ECGs and vital signs, and transmit it in real time to another care provider. That professional can then provide a diagnosis and clinical decision support as well as transport instructions back to the site. Data from multiple patients can be securely viewed via a web browser on scene, during transport or when preparing to receive the patient on handover.25,26 Outsourcing and collaborating to build a stronger system together Taking advantage of innovative business models and outsourcing is another powerful method for extending capacity and reducing operational burdens. As-a-service, fee-per-study and outcome-based models are becoming more common, alleviating staffing shortages and reducing financial burdens. Philips managed services allow hospital teams, for example, to outsource some of their IT management, enabling them to focus their efforts on patient care. When you work alongside our collaborative teams, we can help pinpoint areas for improvement and create results that matter to your organizational goals. Our approach starts with listening to and learning from you, working together to identify the root cause of the challenges you are facing. Our aim is always to recommend clinical, operational and technical solutions tailored to your needs because, as we all know, healthcare transformation is not one-size-fits-all. We take a holistic and longer-sighted approach to our relationship with you, looking for innovative, future-proof ways we can help your teams now and over time.

Agility at hand Philips handheld and tele-ultrasound system recently received FDA clearance to provide COVID-19 diagnostic insight for frontline care providers. With the ability to take images right at the point of care, providers don’t need to transfer patients around the hospital. This helps reduce the risk of transmission to other patients and staff.27
Don't have time to read the guide now? Download a PDF
Summary
Traditional models of care delivered via centralized healthcare systems are vulnerable to capacity challenges, as the recent crisis has laid bare. The heavy burdens of chronic illness, the urgent need to extend healthcare access and the mounting stress healthcare teams feel are constant concerns. But in this moment of crisis lies a crucial opportunity to build a stronger and more resilient healthcare system for a stronger America. That opportunity calls for us to re-envision what healthcare looks like not just in the hospital, but in patients’ communities and homes. It is focusing on prevention and wellness – on ‘never admissions’ where patients are educated and supported to manage their care at home. It is finding innovative ways to support care providers in the hospital so the experience is better for them and their patients. And it is using artificial intelligence to free up the expertise of care providers by eliminating tedious tasks and connecting medical records and data sets to allow care to be extended outside of the hospital walls and reach patients at every step of their journey. Through a unique understanding of clinical issues and continuous collaboration with customers, Philips is well positioned to provide the connected care solutions that are already making this vision a reality. Doing so requires us to share both rewards and risks. At Philips, partnership is far more than a buzzword. True partnership means rolling up our sleeves and working with our customers to identify and implement meaningful solutions customized to each organization’s needs and challenges. To help build stronger healthcare systems, we’re publishing a series of guides that offer strategies, tactics and resources. This is the second of four guides – others focus on optimizing clinical and operational workflows and achieving robust interoperability and cybersecurity. Sign up for updates and to be notified when the next guide becomes available.
Results from case studies mentioned here are not predictive of results in other cases. Results in other cases may vary.
Get the full story
See our resource page and explore the three critical areas government agencies can address today in order to thrive!
References
1. Hartnett KP, Kite-Powell A, DeVies J, et al. Impact of the COVID-19 pandemic on emergency department visits — United States, January 1, 2019–May 30, 2020. MMWR. 2020;69(23):699-704. 2. Goran SF. A second set of eyes: An introduction to tele-ICU. Crit Care Nurse. 2010;30(4):46-55. 3. Chuang C-H, Tseng P-C, Lin C-Y, Lin K-H, Chen Y-Y. Burnout in the intensive care unit professionals. Medicine (Baltimore). 2016;95(50):e5629. 4. https://www.census.gov/content/dam/Census/library/publications/2017/acs/acs-36.pdf 5. RAND Health. Current and Projected Characteristics and Unique Health Care Needs of the Patient Population Served by the Department of Veterans Affairs; 2015. 6. Krumholz HM. Where have all the heart attacks gone? The New York Times. April 6, 2020. Accessed June 20, 2020. https://nyti.ms/2UN1tNN 8. Frost & Sullivan. Telehealth—A Technology-Based Weapon in the War Against the Coronavirus, 2020. K488-48; April 2020. 10. Sutter Health. Patient stories: video visits and COVID-19 response. Accessed June 20, 2020. https://www.sutterhealth.org/patient-stories/video-visits-covid-19-response 13. https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5196 14. Angus DC, Kelley MA, Schmitz RJ, et al. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease. JAMA. 2000;284(21):2762-2770. 15. Castlight Health/The Leapfrog Group. Intensive Care Unit Physician Staffing; 2016. 17. Fortis S, Sarrazin MV, Beck BF, Panos RJ, Reisinger HS. ICU telemedicine reduces interhospital ICU transfers in the Veterans Health Administration. Chest. 2018;154(1):69-76. 18. Lilly CM, McLaughlin JM, Zhao H, et al. A multicenter study of ICU telemedicine reengineering of adult critical care. Chest. 2014;145(3):500–507. 19. Make B, Dutro MP, Paulose-Ram R, et al. Undertreatment of COPD: a retrospective analysis of US managed care and Medicare patients. Int J Chron Obstruct Pulmon Dis. 2012;7:1-9. 20. Dhamane AD, Moretz C, Zhou Y, et al. COPD exacerbation frequency and its association with health care resource utilization and costs. Int J Chron Obstruct Pulmon Dis. 2015;10:2609-2618. 22. Murphy DE, Chaudhry Z, Almoosa KF, Panos RJ. High prevalence of chronic obstructive pulmonary disease among veterans in the urban Midwest. Mil Med. 2011;176(5):552-560. 23. Fried TR, Vaz Fragoso CA, Rabow MW. Caring for the older person with chronic obstructive pulmonary disease: “I was worried that he didn’t have too much room to decline.” JAMA. 2012;308(12):1254-1263. 24. Berry RB, Beck E, Jasko J. Effect of cloud-based sleep coaches on positive airway pressure adherence. J Clin Sleep Med. 2020;16(4):553-562. 26. https://www.usa.philips.com/healthcare/solutions/emergency-care-resuscitation/remote-monitoring